As a dental hygiene clinical instructor, I have observed a significant number of patients not consenting to dental radiographs. Declining dental radiographs can have significant repercussions across several critical areas of dental care. It compromises diagnostic accuracy, impedes effective treatment planning, undermines preventive care measures, poses challenges in upholding legal and ethical standards, and complicates patient education efforts.
Treating patients who have declined necessary dental radiographs can be incredibly frustrating for dental professionals. Without the required diagnostic assessments, we’re essentially working blindfolded, unable to provide the comprehensive care our patients deserve.
When patients decline diagnostic assessments, they leave the clinician to depend solely on visual and tactile methods for detecting pathology. If there is undiagnosed pathology due to the absence of radiographs, the condition will likely deteriorate over time and could lead to significant adverse outcomes.
Reasons for Declining Dental Radiographs
Patients may decline dental radiographs for various reasons. They could worry about radiation exposure, feel anxious about the procedure, face financial limitations, not fully grasp the significance of the radiographs for diagnosis and treatment planning, or simply find the idea of the procedure time-consuming and/or uncomfortable.
Patients may have questions and concerns about the safety of dental imaging procedures. Sometimes, the information they encounter can be misleading, confusing, or incorrect. As a result, patients might refuse to undergo radiography based on information they received from social media or nonprofessional sources.1
In addition, nearly one in four people surveyed (23%) reported encountering financial obstacles to dental care, which led them to avoid visiting a dentist, decline recommended treatments, or both. Approximately 17.3% reported avoiding seeing a dental professional due to cost, and 16.5% stated that they declined recommended dental treatments for the same reason.2
Addressing Patient Concerns
While diagnosing and treatment planning are essential to dental clinicians, these are not the primary concerns of our patients. To effectively change patient behavior, we must address their specific concerns based on their motivations rather than solely focusing on and exerting what we believe is important. One-sided education does not predictably lead to behavior change.3
Motivational interviewing (MI) is a method for influencing various health behaviors and can be effectively applied in dental practice. MI offers a collaborative approach to behavior change in a safe, non-judgmental, and supportive setting, empowering patients to take control of their behaviors.3
MI consists of four processes: engaging, focusing, evoking, and planning. These processes help guide patients toward positive behavior changes. As a patient-centered approach, MI encourages patients to identify their own motivation for change, strengthening the clinician-patient relationship and leading to improved outcomes. Though MI can be challenging for both clinicians and patients, it is a flexible technique that can be successfully implemented in general dental practice.3
Implementing MI includes four aspects:4
- Expressing empathy, which highlights demonstrating an understanding of the patient’s perspective
- Developing a discrepancy between the patient’s current behavior and their important goals or values
- Rolling with resistance and avoiding persuading or arguing
- Supporting self-efficacy and optimism, which aims to give the patient the confidence that they can change
Listen attentively to the patient’s concerns and fears. Empathize with their feelings and reassure them by addressing their specific worries. Establish trust and rapport with the patient by demonstrating professionalism, competence, and compassion. Consider factors such as past experiences and personal beliefs that may influence their decision-making process. A trusting relationship can increase their confidence in accepting dental radiographs.4
Providing patients with accurate details and personalized education about the vital role of radiographs in maintaining oral health is essential. By highlighting how their unique dental history, such as previous dental caries and caries risk, root canal treatments, restorations, dental implants, and periodontal status, necessitates a comprehensive evaluation of each tooth, the importance of utilizing dental radiographs becomes clearer. This tailored approach ensures that the patient understands the necessity of these diagnostic tools in identifying potential issues and devising effective treatment plans specific to their needs.1,4
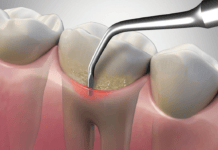
Utilizing visuals, such as intraoral photos, dental models, or videos, in the explanation process provides tangible visual evidence of the potential risks associated with not undergoing assessment modalities needed for diagnosis and treatment. These visual aids allow patients to see firsthand any existing dental issues, such as dental caries, infections, or bone loss, that may not be apparent during a regular visual examination. By presenting this information visually, patients can better grasp the importance of timely diagnosis and treatment in preserving their oral health and preventing further complications.5
Create a safe and supportive environment where patients feel comfortable sharing their concerns openly. Encourage them to ask questions and express any uncertainties they may have.4
Offer reassurance by explaining the safety measures in place that minimize radiation exposure, such as:6
- Using digital imaging instead of conventional film
- Restricting the beam size to the area that needs to be assessed (i.e., rectangular collimation) and properly positioning patients so that the most diagnostic image can be taken
- Incorporating CBCT only when lower-exposure options will not provide the necessary diagnostic information
- Adhering to all applicable federal, state, and local regulations on radiation safety
Patient Autonomy
Respecting the patient’s autonomy is essential. Patients, along with their guardians or substitute decision-makers, possess the right to either consent to or decline radiographs. Finding out exactly why they refuse radiographs and addressing their concerns can help clinicians and patients make informed decisions together.7
If a patient still refuses radiographs after addressing questions and concerns, they can sign an informed refusal form. The American Dental Association (ADA) states, “Accepted refusals should be well-documented, with a clinically-supportable rationale, and a plan for gathering necessary diagnostic information within a reasonable time frame.”7
However, signing an informed refusal form essentially entails patients consenting to treatment that falls below the accepted standard of care and does not release a clinician from liability.7 The ADA states, “Dentists are recommended to not take on this risk and to recognize that the patient cannot “release” the dentist from potential liability for failure to diagnose by signing a waiver of liability. Of course, there are many variables involved, but routinely accepting patient refusals for radiographs can lead to non-defensible claims and/or lawsuits.”7
If the dentist believes that the refusal compromises their ability to accurately diagnose and/or provide appropriate treatment, they have the right to decline to provide compromised care as requested by the patient and dismiss the patient from their practice.7,8
In Closing
Effectively addressing patient objections is crucial to safeguarding the health of our patients and upholding professional standards. Customize your approach to address the specific needs and preferences of each patient. What works for one patient may not work for another, so it’s essential to adapt your communication style accordingly.
Respect the patient’s right to make informed decisions about their own health care. Avoid pressuring them. Instead, focus on providing information and support to help them make the best decision for themselves. After the discussion, follow up with the patient to see if they have any further questions or concerns.
By demonstrating empathy and understanding, dental professionals can build trust and rapport with patients, leading to improved communication, increased patient satisfaction, and better outcomes in dental radiograph acceptance, hence better dental care.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Al Faleh, W., Bin Mubayrik, A., Al Dosary, S., et al. Public Perception and Viewpoints of Dental Radiograph Prescriptions and Dentists’ Safety Protection Practice. Clinical, Cosmetic and Investigational Dentistry. 2020; 12: 533-539. https://doi.org/10.2147/ccide.s281851
- Thompson, B., Cooney, P., Lawrence, H., et al. The Potential Oral Health Impact of Cost Barriers to Dental Care: Findings from a Canadian Population-Based Study. BMC Oral Health. 2014; 14: 78. https://doi.org/10.1186/1472-6831-14-78
- Gillam, D.G., Yusuf, H. Brief Motivational Interviewing in Dental Practice. Dentistry Journal. 2019; 7(2): 51. https://doi.org/10.3390/dj7020051
- Ramseier, C. A., & Suvan, J. E. (Eds.). (2010). Health Behavior Change in the Dental Practice. Wiley-Blackwell.
- Thorat, V., Rao, P., Joshi, N., et al. Role of Artificial Intelligence (AI) in Patient Education and Communication in Dentistry. Cureus. 2024; 16(5): e59799. https://doi.org/10.7759/cureus.59799
- Benavides, E., Krecioch, J.R., Connolly, R.T., et al. Optimizing Radiation Safety in Dentistry: Clinical Recommendations and Regulatory Considerations. Journal of the American Dental Association. 2024; 155(4): 280-293.e4. https://jada.ada.org/article/S0002-8177(23)00734-1/fulltext
- Radiographic Imaging. (n.d.). American Dental Association. https://www.ada.org/en/resources/practice/practice-management/radiographic-imaging
- Frequently Asked Questions – Dental Radiographs. (n.d.). Royal College of Dental Surgeons of Ontario. https://www.rcdso.org/en-ca/standards-guidelines-resources/rcdso-news/frequently-asked-questions/information-on-dental-radiographs