Tetracycline and minocycline are common antibiotics used medically for infections and inflammation. While useful for medical reasons, dental professionals know it more for internal staining of the teeth.
Tetracyclines lead to permanent tooth staining when ingested during pregnancy, nursing, or during the developmental period of secondary and primary teeth. This vulnerable time frame is from the fourth month in utero through the fifth month of postpartum. The overall prevalence of tetracycline staining is 3% to 4%. With minocycline, the prevalence is 3% to 6%.1
Tetracycline
Tetracycline is an antibiotic to treat several gram-negative and gram-positive infections. It’s common uses are for acne, cholera, plague, malaria, mycoplasma, chlamydia, and syphilis. Although it has positive use systemically, it also has adverse effects dentally. It may cause tooth discoloration on primary and permanent teeth depending on the length of treatment or exposure, the dosage, and the stage and degree of mineralization.
Permanent teeth tend to appear less intense but more diffused than primary teeth. When the teeth are exposed to tetracycline, calcium ions are binding to the teeth during the mineralizing or calcifying process of development. This antibiotic settles into the calcium that’s used to develop teeth. Tetracycline is absorbed into the teeth through the blood, which travels to the coronal of the pulp then to the subodontoblastic area before settling into the predentin. If this happens before the teeth erupt, the tetracycline binds to calcium ions, causing the initial yellow coloring.
Newly erupted teeth present with a bright fluorescent yellow band, and once exposed to sunlight, the tetracycline crystals in the teeth undergo a photochemical reaction and oxidizes. With this process, a gradual change of color changes from yellow and darkens to a nonfluorescent brown, grey, or red-brown hue over a period of months to years.
Since the anterior teeth are exposed to sunlight, it dramatically changes to darker colors. The molars are not exposed to sunlight, so they tend to be lighter in color. This discoloration is permanent. Regardless of the severity of the staining and aesthetic appearance, the tooth’s health is not compromised.2
While the risk of tetracycline discoloration is highest in children, it is advised that pregnant women after the fourth month and children up to eight years of age avoid tetracycline. The teeth are most prone during calcification with the primary teeth up to 10 to 14 months.2 The permanent anterior teeth can be affected from six months to six years, and the permanent posteriors up to eight years and are usually found in the gingival third of the crown.
The degree of discoloration is in relation to the dose and duration of exposure to tetracycline. This occurs more often when accumulative doses exceed three grams, or the use of the antibiotic is longer than ten days.3 When tetracycline is administered in cycles, discoloration is usually band-like compared to extended use of tetracycline where results are more of a homogeneous appearance.
Degrees of discoloration are based on the extent and degree of use.
First degree: Light yellow, grey, or brown. Confined to incisal three-quarters without banding
Second degree: Darker and more uniform discoloration without banding
Third degree: Very dark blue or grey with banding4
Fourth degree: Intense pigmentation combing very dark stains with highly pronounced bands4 (see Figure 1)

Minocycline
Minocycline is a semisynthetic tetracycline derivative and is used as a second-line drug for those with penicillin allergies. It is a broad-spectrum antibiotic commonly used in the long-term treatment of acne vulgaris, rosacea, and rheumatoid arthritis. It is also widely used to treat a variety of bacterial infections, including urinary tract infections, respiratory infections, skin infections, chlamydia, gonorrhea, syphilis, tick fever, and several others.5,6
Since minocycline is used during all ages, some noteworthy adverse effects are worth knowing. It lessens the effect of birth control pills, causes fetal harm, and passes into breast milk, affecting bone and tooth development in a fetus or nursing baby.5
In more severe cases, it can cause a skin rash that can become fatal. If this medication is used after its expiration date, it can cause kidney damage. Taking iron supplements, calcium, antacids, or laxatives within two hours of taking minocycline can lessen its effect. Do not take if allergic to this antibiotic or similar antibiotics such as demeclocycline, doxycycline, or tetracycline.5
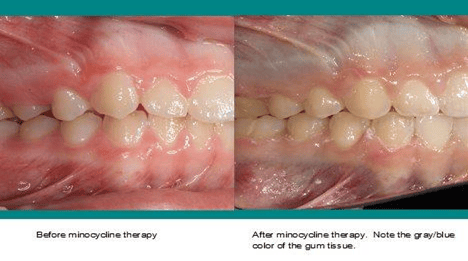
With minocycline being prescribed for multiple infections, it covers a wide range of ages. So the chances of tooth discoloration continue throughout life. This discoloration is a distinct blue-gray band, commonly found in the incisal and middle third of the crown (see Figure 2). It does not fluoresce under UV light as tetracycline does.1

This discoloration is in relation to longer durations and higher doses of minocycline use. Its route of process is different than tetracycline in contributing to teeth staining. While tetracycline is calcium involved, minocycline is protein involved with both an intrinsic and extrinsic theory.
The intrinsic theory happens upon absorption. Minocycline is protein driven in the blood and binds to high collagen-containing tissue such as teeth and bone to cause discoloration.
The extrinsic theory happens when the surface of the teeth meets minocycline. The saliva holds onto concentrations of this antibiotic and stays in the gingival crevicular fluid. Since this fluid remains at the gumline, the high concentration of minocycline in the saliva soaks into the enamel where the minocycline oxidizes when it is exposed to oxygen or bacteria.
Minocycline has been associated with discoloration of bones, oral mucosa, skin, sclerae, and nail beds7 (see Figure 3).
Other Teeth-Staining Tetracyclines
Tigecycline − Tigecycline is a glycylcyline derivative and is also a broad-spectrum antibiotic. It has a lower susceptibility to resistance compared to other antibiotics. They are commonly used for digestive and skin infections. It also crosses the placenta, and, if taken during the second and third trimester, it may cause a yellow-gray-brown discoloration of the teeth.3
Oxytetracycline − Oxytetracycline is the second tetracycline to be identified and is a broad-spectrum antibiotic. It works by interfering with the ability of bacteria to produce essential proteins. Without these proteins, bacterial growth is inhibited. It’s used to treat a variety of bacterial infections such as acne and chlamydia. The brand name is Terramycin, which is no longer available in the United States (but generic versions are still available).
Tooth discoloration of yellow, brown, or gray occurs when used within the second and third trimester during pregnancy, during nursing, or during childhood under the age of eight.4
Chlortetracycline − Chlortetracycline is the first tetracycline to be identified. This antibiotic produces a slate gray if used during pregnancy.4
Whitening Tooth Stain
Intrinsic staining is endogenous staining that has been incorporated into the tooth matrix.
Generalized intrinsic staining is indicative of disruption during tooth development. Localized intrinsic staining usually occurs before or after teeth have erupted. A number of metabolic and systemic factors affect the dentition and cause the inner tooth discoloration.6
Whitening tetracycline stain is possible, but it all depends on the initial color and consistency. Nonstained teeth average three to six weeks with whitening trays, while tetracycline-stained teeth may take two to 12 months for results.
Initially, a slight change may occur within the first few days and then stabilize for a month and pick back up to achieve their maximum result. It won’t necessarily “whiten” the teeth, only lighten the shade. The teeth will reach an endpoint or plateau to whitening that is determined by the composition of the teeth and not by the whitening product or technique.8
Whitening is most effective during the first and second degrees of discoloration. Gray discolorations are the most challenging to whiten while brown and yellow discolorations are more receptive.
The gingival area is the most difficult to whiten with tetracycline-stained teeth since the tooth color arises from the dentin where the tetracycline molecule is tightly bounded. The darkest teeth at the cementoenamel junction, especially blue-gray discoloration, have the poorest prognosis for full lightening. Discoloration in the incisal third has the best prognosis.
When using bleaching trays, 10% carbamide peroxide is the most effective in results with tetracycline stain.8
Tooth Stain Treatment
If the tetracycline stain is too severe and whitening is not viable, other treatment options are available. Since tetracycline staining is common with the anterior teeth, aesthetics is very important. Restorations such as veneers, crowns, and composite bonding to cover the stain are a more routine treatment.9
Aggressive preparation of the teeth is necessary before placing a restoration. With this challenge to mimic a natural tooth, preparation of removing as much underlying darkness of the tooth as possible is needed for a good result for the translucent effect of porcelains. Bleaching the tetracycline-stained tooth may be the first option to see how well it lightens the tooth. The lighter the tooth encourages the more successful of an outcome with veneers or crowns. If the tooth doesn’t lighten enough for a positive result in placing a restoration, then removing healthy enamel is the other option. In the area of a dark band, the degree of darkness and the choice of restoration will determine the aggressiveness of tooth preparation.
A more aggressive approach, though, may be elective endodontic therapy with internal bleaching. However, removing a healthy pulp for aesthetics is not usually advised.9
Antibiotic-induced tooth discoloration is rarer now than previously since these antibiotics are less likely to be prescribed to children or pregnant women. With the adverse drug reaction, it can create esthetic and psychological self-esteem issues. Dental professionals can offer advice and treatment options to the patient.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Busti, A. The Mechanism for Minocycline (Minocin, Dynacin, Solodyn) Associated Staining of the Teeth and How is it Different from Tetracycline. Evidence-based Medicine Consult. October 2015. Retrieved from https://www.ebmconsult.com/articles/minocycline-stains-teeth-different-tetracycline.
- Busti, A.J. The Mechanism for Tetracycline Associated Staining of the Teeth. Evidence-based Medicine Consult. October 2015. Retrieved from https://www.ebmconsult.com/articles/tetracycline-stains-teeth-mechanism.
- Kadam, A., Ganachari, M., Mahendra Kumar, B., Gurunath, S. Drug Induced Tooth Discolouration. The Internet Journal of Dental Science. 2008; 7(2). Retrieved from https://ispub.com/IJDS/7/2/10979.
- Thomas, M.S., Denny, C. Medication-Related Tooth Discoloration: A Review. Clinical Dentistry. 2014; 41(5): 440-2, 445-7. Retrieved from https://www.researchgate.net/publication/264393077_Medication-related_tooth_discoloration_A_review.
- Minocycline. Drugs.Com Retrieved from https://www.drugs.com/minocycline.html.
- Raymond, J., Cook, D. Still leaving stains on teeth-the legacy of minocycline? Australas Med J. 2015; 8(4): 139-142. doi:10.4066/AMJ.2015.2335.
- Johnston, S. Feeling blue? Minocycline-induced staining of the teeth, oral mucosa, sclerae and ears – a case report. Br Dent J. 2013; 215: 71–73. Retrieved from https://doi.org/10.1038/sj.bdj.2013.682.
- Mrazek, B. Don’t bleach until you see the white of their eyes. Compend Contin Educ Dent. 2004; 25(6): 472-476.
- Basset, J., Patrick, B. Restoring Tetracycline-Stained Teeth with a Conservative Preparation for Porcelain Veneers: Case Presentation. Practical Procedures & Aesthetic Dentistry. 2004; 16(7): 481-486.











