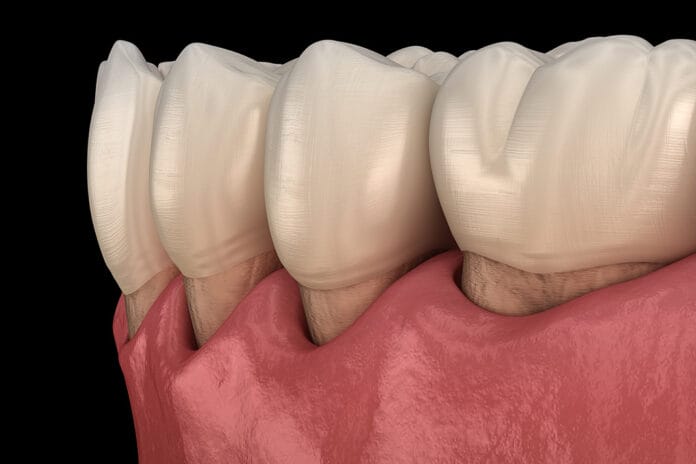
Recession is a common gingival tissue problem resulting from the apical migration of the marginal gingiva.3 As presented by Mercado et al., gingival recession is highly prevalent throughout the worldwide adult population, ranging in incidence from 30% to 100%.2 This results in the exposure of the root structure, often leading to sensitivity and creating an increased risk for cervical decay.3 Etiologies of recession include “plaque-induced inflammation, mechanical abrasion, and trauma.”2
When apical migration has advanced toward or passed the mucogingival junction, a mucogingival defect becomes present and is in need of treatment. Tissue regeneration is necessary for the treatment of severe gingival recession and can be completed in several forms.3
Subepithelial Connective Tissue Graft
Soft tissue grafting includes free gingival grafting, connective tissue grafting, and laterally positioned grafting. According to Weinberg et al., when focusing on an isolated tooth or multiple adjacent teeth and aiming for root coverage, a subepithelial connective tissue graft (SCTG) is “the procedure of choice.”
Langer and Calagna initially presented the procedure in 1982. This style of grafting enjoys several advantages including, “(1) There is no open wound on the palate as in a free gingival graft, (2) the graft has a better blood supply coming from both the underlying connective tissue and the overlaying flap, and (3) better aesthetics and tissue and color blend are seen.”3 Mercado et al. also discusses the procedure as the “gold standard” due to the procedure’s consistency in outcome, aesthetic achievement, and attainment of increased keratinized tissue width.2
For this procedure to be completed, there must be adequate donor tissue available. If there is inadequate donor tissue, the procedure will be contraindicated, and a free gingival graft with donor tissue from a separate site such as the palate is likely more ideal. Because donor sites of the free gingival grafts heal by secondary intention (meaning an open wound), an SCTG is a less painful treatment option in the treatment of advanced gingival recession when indicated and accessible with adequate tissue.3
Technique ─ Guidelines presented by Weinberg et al. begin with the clinician providing local anesthetic. A “split-thickness flap” is then “raised at the recipient site using a surgical blade.” Next, “a flap is raised at the donor site on the palate, and connective tissue is harvested while leaving the epithelium on the outside of the flap. This palatal flap is sutured into place. The connective tissue is placed on the recipient site and sutured in place with absorbable sutures. A periodontal dressing may be applied.” After the procedure is completed, the clinician shall provide post-operative instructions.3
Post-operative instructions ─ The instructions provided would include directing the patient to avoid smoking and avoid brushing the dressed area for one to two weeks until the periodontal dressing is removed. At the post-operative evaluation appointment, the dressing and sutures will be removed. Depending on the patient’s healing, the clinician may choose to redress the area and have another evaluation in an additional week.
After adequate healing and removal of the dressing, the patient may begin light brushing using the “roll technique.” The patient should avoid contact with the gingiva and, in the event of bleeding, should discontinue brushing and just rinse the area using warm water. Regular brushing and interdental cleaning should not be completed until ideal healing is seen by the oral practitioner. Because root exposure is expected in this procedure, the area should be re-evaluated in six months once the clinician is satisfied with healing at post-operative appointments.3
Additional Factors Affecting Treatment
To expand on the indications for this type of procedure, one may be interested in a multi-factorial case involving wear of the incisal edges of teeth and gingival recession. These signs of dental trauma are often due to parafunctional habits like clenching and grinding. When restoring the incisal edges for a patient with such conditions, a clinician should also address the gingival attachment. In the study, “Subepithelial connective tissue graft conjugated to minimally invasive ceramic laminates—1 year follow-up,” authors Costa et al. address the results of bruxism and how providing treatment for both the incisal edges of the teeth as well as the gingival margin, treats the entire problem of occlusal trauma and the resulting recession.1
One of the main problems associated with gingival recession ─ especially in those with a damaging parafunctional habit ─ is dentinal sensitivity. Other problems associated with bruxism include “morphological and altered size of the teeth caused by gingival recession and incisal wear.” The authors, Costa et al., established their report to address these problems with the combination of subepithelial connective tissue grafting and minimally invasive ceramic laminate veneers. Their procedure involved the SCTG first to provide treatment of the exposed root surfaces. Once healing was completed, the veneers were placed to provide a more pleasant aesthetic appearance and restoration of the damaged tooth structures.1
A clinician who has treated a patient with bruxism would question how veneers, even with the addition of SCTG, will provide treatment for these specific patients in the long-term aspect, as bruxism does not just disappear once a treatment such as this is completed. The authors knew this as well and provided a “multidisciplinary planning of treatment” to address future complications. They chose ceramic laminate veneers that are more durable to bruxism, avoiding severe wear in the future, as well as utilized the science of myorelaxant plaques. These guards, worn over the teeth, are used “to reduce future dental wear that can directly affect the teeth and surrounding tissues.” They “maintain the restorative work and decrease muscle activity.” This will allow for the teeth to remain in good condition as well as provide the temporomandibular joint the opportunity to relax and decrease “the frequency of bruxism.”1
Whether a patient is in need of gingival grafting for a single tooth or multiple adjacent teeth, possibly in conjugation with dental hard tissue restoration, a subepithelial connective tissue graft is an ideal choice. Due to the procedure’s high predictability, ideal aesthetic appearance upon healing, and ideal blood supply and closed tissue healing, an SCTG is the “gold standard” for treating severe gingival recession leading to a mucogingival defect. Clinicians should be knowledgeable of this procedure’s value to patients in addition to its ideal use with the pairing of ceramic laminate veneers and occlusal therapy in the treatment of bruxism, one of the main causes of gingival recession.
Need CE? Click Here to Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Costa, L.C.M., Zica, J.d.S., da Costa Junior, A.R.d., Machado, L.S., Lacerda, L.H.C., Morgan, L.F.d.S.A. Subepithelial Connective Tissue Graft Conjugated to Minimally Invasive Ceramic Laminates—1 Year Follow-up. Journal of Esthetic and Restorative Dentistry. 2020; 32(4). Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1111/jerd.12585
- Mercado, F. Hamlet, S., Ivanovski, S. A 3-year Prospective Clinical and Patient-centered Trial on Subepithelial Connective Tissue Graft with or without Enamel Matrix Derivative in Class I-II Miller Recessions. Journal of Periodontal Research. 2019; 55(2). Retrieved from https://pubmed.ncbi.nlm.nih.gov/31808142/
- Weinberg, M.A., Westphal Teile, C.M. Froum, S.J., Segelnick, S L. (2015). Principles of Periodontal Surgery: Gingivectomy, Osseous Resection, and Periodontal Plastic Surgery. In Comprehensive Periodontics for the Dental Hygienist (4th, pp. 348-375). Pearson.