Periodontitis is one of the most widespread preventable diseases in the world. A vast majority of studies, both qualitative and quantitative, looked at the association between periodontal disease and osteoporosis in geriatric populations. But what about the occurrence of periodontal disease and osteoporosis in adults that are currently determined to be ‘middle-aged’? Are the two conditions related to someone that young?
The Association between Bone Mineral Density and Periodontal Disease in Middle-Aged Adults looked at 7298 adults between the ages of 40 and 44. The researchers state, “To our knowledge, the relationship between osteoporosis and periodontal disease in young adults is rarely addressed and difficult to establish due to the association being confounded by other factors such as gender, hormone intake, smoking, race, and age.”
Silent Osteoporosis in Early Age
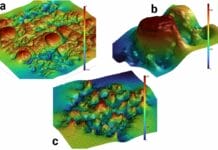
Low bone density and deteriorated microarchitecture of bone tissue, or osteoporosis, weakens a person’s skeletal structure. The creation of bone tissue slows while the disintegration of older bone increases in speed. The bone is simply unable to keep up with demand. “Wowern et al. revealed that severe osteoporosis, which significantly reduces the bone mineral content of the jaws, may be associated with a less favorable attachment level in the case of periodontal disease. Since the loss of alveolar bone is a prominent feature of periodontal disease, severe osteoporosis is suspected of being an aggravating factor in the case of periodontal disease.”
Men and women can both suffer from osteoporosis, but women are naturally more prone due to the chemical makeup of their bodies. Most people are simply not tested early enough. Women are routinely checked for this disease as soon as menopause hits, but men usually need to show more advanced symptoms before the disease is actually noticed.
Osteoporosis can become more common as age increases and increases in intensity the longer it is ignored. Many women don’t think about and are not tested for osteoporosis during their thirties and forties because patients and doctors see the disease as a geriatric problem.
Women are more at risk for severe osteoporosis than men due to normal hormonal fluctuations, and the problems that this disease causes can show up earlier than we think. There are sometimes no signs of early osteoporosis, which is why doctors don’t think about it being a problem until a person’s later years.
This is just another example of how dental professionals can notice the early symptoms of a disease that their patient or primary care physician doesn’t see. We have the chance to increase their dental-related quality of life as well as the stability of their long-term health and comfortability.
The Study Results and Discussion
The researchers found a significant correlation between bone mass density and periodontal disease; the lower the bone mass density, the higher the incidence of periodontal disease. In this study, low bone mass was associated with a 13% increase in the risk of periodontal disease.
The researchers’ state:
- “The relationship between osteoporosis and periodontal disease may be supported by three mechanisms that have been mentioned (in previous research), comprising systemic to local bone resorptive disease, hormonal impact on bone homeostasis inflammation, and inflammation and bone homeostasis.”
- “Osteoporosis of the alveolar bone may lower the resistance of the periodontium to infectious challenge and may result in a local infection of the periodontium that first invades the cortical bone and results in a dimensional change in the alveolar ridge.”
- “However, a non-infectious mechanism was also considered to be a possible mechanism, since the association between alveolar bone resorption and tooth loss has been shown to be stronger than other clinical measurements of periodontal disease.”
- “Another possible mechanism involves inflammatory cytokines, in that osteoporosis patients have elevated systemic levels of pro-inflammatory cytokines IL-1, IL-6, and TNF-α. These cytokines account for osteoclastogenic bone resorption-inducing cytokines and are also involved in the tissue response to periodontal disease.”
- “Moreover, homeostatic bone remodeling involves “physiologic inflammation” to recruit non-phlogistic macrophages for the clearance of apoptotic bone cells. Interestingly pro-resolving lipid mediators (SPMs) have been unveiled as contributors to an active process of inflammation and are involved in bone homeostasis.”
In closing, the researchers state, “…whether there is causation between the two conditions is still elusive, in terms of whether osteoporosis causes periodontal disease or vice versa. More studies are required. However, our study was based on a large community-based data set and targeted young adults. We believe that our result could be used as a warning to raise public awareness about osteoporosis and periodontal disease in young adults.”