Many systemic disorders have symptoms present in the mouth, sometimes before symptoms are present elsewhere in the body. Cardiovascular, psychosomatic, gastrointestinal, renal, and endocrine disorders are a few that can make themselves known in the mouth before showing up in the traditional ways. We may observe oral symptoms of eating disorders before our patients have been diagnosed, or in the case of children before their parents realize that there is a problem.
An eating disorder can be irreparably damaging and even deadly to its victims. Early recognition may save a life, and there may be other non-oral symptoms that we notice to support or validate our worries before sharing any concerns.
Oral Cavity and Eating Disorders: An Insight to Holistic Health is a comprehensive guide on many of the oral symptoms of eating disorders, or ED, particularly anorexia and bulimia specifically, as they are the most common categories of this type of eating disorders.
Eating Disorders
Anyone can develop an eating disorder, but the disease occurs mostly in females between the ages of 16 and 25. Symptoms can appear in pre-teens and early teen years as well, and they are serious.
Dental Erosion
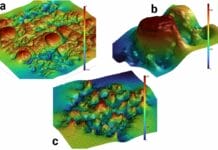
Erosion refers to the gradual destruction of tooth structure. This is not necessarily caused by bacteria but by a chemical reaction. This is easily noticeable as the teeth start to flatten and develop cup-shaped lesions.
The location of the erosion can tell you whether the acidic, chemical wearing of teeth comes from stomach acid or foods and/or beverages ingested. The researchers stated, “Initially, it appears as soft smooth-shining glossy tooth surfaces; gradually progressing to flat or superficial, flat indentations, coronal to the cementoenamel junction. Advanced lesions appear as cup-shaped defects on the occlusal/incisal aspects of the tooth, with markedly altered tooth morphology. Holst and Lange (1939) coined the term ‘perimylolysis’ and refers to palatal erosions on the maxillary teeth. The mandibular lingual tooth surfaces are usually spared as they are shielded by the tongue and saliva from sublingual and submandibular glands”
Dentinal hypersensitivity is common with dental erosion.
Dental Caries
Caries is the most common side effect of ED. Personal oral hygiene can suffer naturally with depression. Malnutrition alters the composition of saliva and the amount secreted in the mouth. Dehydration and the number of laxatives, appetite suppressants, and diet pills ingested all contribute to increased caries.
The vomiting with bulimia demineralizes tooth structure, leading to high caries risk. Caries is directly related to the severity of erosion that the patients display. Both are affected directly by the chemical makeup of saliva.
Salivary Glands
Chronic sialadenosis is very common, especially among those who suffer from bulimia. The salivary gland is enlarged but not inflamed. This increases acinar protein production and impairs the actual secretion of the saliva into the mouth.
Necrotic sialadenosis occurs in bulimia patients. This enlargement of the salivary glands are inflamed, and the gland necrotizes, causing open sores and painful ulcers.
Anorexic patients may have hyposalivation during their periods of starvation, and bulimic patients will have it during their binges. The disruptions in the amount of saliva can exacerbate lesions and even prevent them from healing.
Gingivitis and Periodontitis
Many patients with an eating disorder do not have the best personal hygiene, especially oral hygiene. ED patients may lack essential vitamin C and suffer from gingival recession due to brushing directly after binging, instead of waiting for pH to rise, then brushing. Malnutrition increases the damage caused by gingivitis and periodontitis.
Oral Lesions
Both stomach acid and malnutrition cause mucosal lesions and ulcers. Chronic oral infections and pale gingiva may be noticeable. The lesions burn and the mucosal areas atrophy, causing pain.
Intraoral Microflora
Both acidogenic and cariogenic microbes are increased in ED patients’ saliva, and the pH balance is more acidic. The saliva’s low pH may lead to or exacerbate erosion, caries, gingivitis, periodontitis, lesions, gland issues, and open sores that increase the chance of infection.
Non-Oral Symptoms
Visually check your patient for dry skin and calluses on their middle and pointer fingers. Get to know your patients as individuals and build rapport. In truly knowing your patients, it is easier to notice weight and complexion changes. This is a very delicate topic that must be addressed carefully and without judgment.
Keep an eye out for thinning hair, drug abuse symptoms, and obsessive-compulsive behaviors, such as nail-biting, over-flossing, and extreme brushing. Are they slow to respond to your requests or seem to lack energy? Are their eyes dilated, or do they seem to be depressed?
Most of the oral problems produced by eating disorders are irreversible. And sometimes, our patients want to stop their negative habits and don’t know how to begin. They need someone to notice them and show delicate support to jumpstart the action. Hygienists and other dental professionals can help stop further damage in its tracks.