Cardiovascular disease has been one of the leading causes of death worldwide for many years. Genetic factors play a role in disease onset and progression, but in addition to specific genetic components, a large body of evidence indicates systemic inflammation may also play a role.1
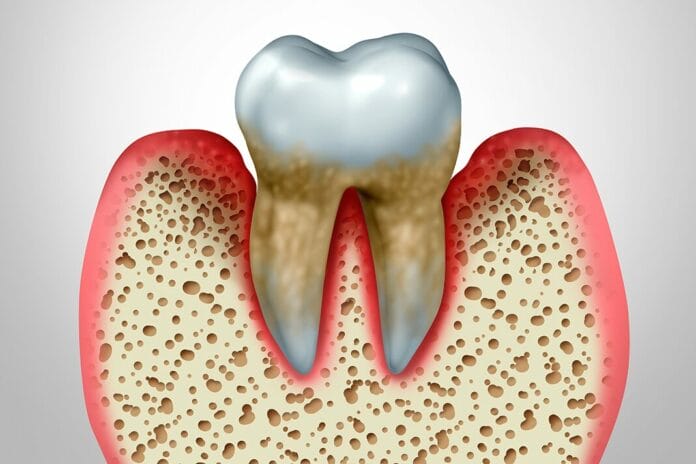
Systemic inflammation is also associated with periodontitis. Periodontitis contributes to systemic inflammation via bacteremia and increased production of inflammatory mediators from compromised gingival tissue into the bloodstream.1
A prospective cohort study investigated the “extent to which periodontitis and systemic inflammation are longitudinally associated with mortality” on a population-based level.1
The Study
The study included 3047 participants. Information and vital signs were collected at different intervals for up to 16.8 years. Periodontal status was determined using pocket probing depths (PPD) and clinical attachment loss (CAL). Calibrated dentists performed all dental examinations.1
The assessed covariates included sociodemographic, behavioral, and obesity-related risk factors. Sociodemographic information was collected via questionnaires, including age, sex, living with a partner, and household income. Behavioral risk factors were also self-reported and included alcohol consumption, smoking status, physical activity, and dental health behaviors. Obesity-related risk factors included body mass index (BMI), diabetes mellitus, and dyslipidemia.1
The Results
A total of 3047 participants were monitored, during which time 380 (12.5%) passed away due to CVD (n=125) or other causes (n=225). At baseline, survivors were significantly younger and female, had better periodontal health and lower inflammatory parameters, and had lower frequency of almost all risk factors.1
An interesting finding was that the proportion of current smokers was higher among survivors than non-survivors. Those who passed away due to CVD were more likely to have diabetes mellitus, less likely to brush their teeth, and had about two fewer teeth than those who passed from other causes.1
There were no significant differences in survival between healthy participants and those with high inflammation levels alone. However, people with severe periodontitis had significantly lower survival compared to healthy participants and those with high inflammation alone. The shortest survival was seen in people with both high inflammation and severe periodontitis.1
When researchers used advanced models to account for changes over time and other factors, they found that all inflammation markers were associated with a higher risk of all-cause mortality.1
Each 1-point increase in the periodontitis score was associated with a 40% higher risk of all-cause mortality. Similarly, each 1-point increase in the inflammation score was associated with a 35%–39% higher mortality risk. When combined, periodontitis and inflammation added extra risks: a 19% higher risk of mortality from all-cause and a 28% higher risk of mortality from CVD. However, there was no evidence of the effect of periodontitis mediated by inflammation and vice versa.1
This study had several limitations, including a lack of detailed information on previous periodontal treatments. Participants were asked about periodontal treatment in the last five years. Still, the validity of the information was a concern as many participants displayed confusion regarding the difference between prophy and periodontal treatment. Additionally, there was a risk of recall bias as the participants were self-reporting. There was also concern for recall bias as some of the information on non-fatal CVD events was self-reported as well.1
Conclusion
Both periodontitis and systemic inflammation were significantly associated with all considered types of mortality in this study. When combined, they added extra risks: a 19% higher chance of death from any cause and a 28% higher chance of mortality from CVD. However, the association of how these two conditions influence each other was marginal, and the methods used in this study couldn’t fully measure their combined impact.1
The researchers conclude that the synergistic effect of periodontitis and systemic inflammation on mortality emphasizes the importance of interprofessional collaboration between health care professionals to manage these risks and improve overall health. The possibility of CVD risk reduction through treating periodontitis is worth exploring, especially for people who have both periodontitis and high levels of systemic inflammation.1
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
Reference
- Pink, C., Holtfreter, B., Völzke, H., et al. Periodontitis and Systemic Inflammation as Independent and Interacting Risk Factors for Mortality: Evidence from a Prospective Cohort Study. BMC Med. 2023; 21(1): 430. https://pmc.ncbi.nlm.nih.gov/articles/PMC10642059/