The immune system’s ability to remember past encounters with threats like bacteria and viruses is a remarkable asset. However, this immune memory can have both positive and negative effects. While it can be beneficial in fighting off infections, chronic inflammation can lead to a misguided immune response, perpetuating inflammatory conditions.
A study published in the journal Cell describes how innate immune memory can contribute to the development of inflammatory systemic conditions and the association with periodontitis.1
The Study
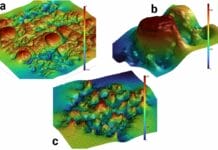
Researchers explored the mechanism behind innate immune memory’s impact and enhanced risk of systemic inflammatory conditions in patients with periodontitis. Specifically, they focused on the association between periodontitis and arthritis. The study revealed that alterations to immune cell precursors in the bone marrow could cause one inflammatory condition to increase susceptibility to another.1
The Results
The researchers set out to determine if the association between comorbidities, such as periodontitis and arthritis, could be linked to the innate immune training occurring in the bone marrow. They found that myeloid cells and their progenitors in the bone marrow expanded within a week of inducing periodontal disease in mice. Interestingly, even after resolving the periodontitis, these progenitor cells retained an inflammatory memory encoded in their epigenetic changes, which altered gene expression patterns upon future challenges.1
Previous work by researchers has shown that the innate immune system’s myeloid cells, including neutrophils and macrophages, also possess the ability to “remember” past encounters, becoming more responsive when encountering new threats. This innate immune memory was found to be encoded in the bone marrow, and its effects could be transferred through bone marrow transplants.1
Understanding the interplay between oral health and systemic inflammatory conditions has become increasingly important as research continues to emerge indicating oral-systemic associations. Yet, there is “no unifying casual mechanism of how periodontitis affects and is affected by comorbidities.”1
This research suggests that chronic gingival inflammation could have broader implications for overall health, making it crucial for early detection and effective management of periodontitis.1
Moreover, this study provides insight into the role of bone marrow in immune memory and the potential implications for bone marrow transplant recipients. Donors with underlying inflammatory conditions could transfer detrimental immune memory to the recipients, leading to an increased risk of inflammatory disorders. This information may prompt a reevaluation of bone marrow donor selection protocols.1
Conclusion
In summary, the immune system’s memory can significantly impact our health, both positively and negatively. The link between periodontitis and systemic inflammatory conditions like arthritis underscores the importance of oral health in overall well-being. Early detection, prevention, and appropriate management of periodontitis may help mitigate potential systemic health risks associated with chronic inflammation.
As dental professionals continue to play a vital role in promoting oral health, ongoing research in the field of immunology can aid in providing comprehensive and patient-centered care for individuals seeking to maintain optimal oral and systemic health.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
Reference
- Li, X., Wang, H., Yu, X., et al. Maladaptive Innate Immune Training of Myelopoiesis Links Inflammatory Comorbidities. Cell. 2022; 185(10): 1709-1727.E18. https://doi.org/10.1016/j.cell.2022.03.043