Disclosure: We value transparency at Today’s RDH. This quiz is sponsored content from Dentsply Sirona Preventive as part of our sponsored partner program.
Let's test your dental aerosol knowledge!
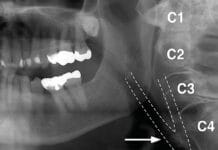
Oral bacteria have been detected in aerosols produced by dental procedures as far as 6.5 feet from the procedure field (patient’s mouth).
“Most procedures performed by the dental team have the potential for creating contaminated aerosols and splatter. Aerosols are tiny particles or droplets which remain suspended in air. These aerosols represent an infection hazard due to their gross contamination with microorganisms and blood. A fourfold increase of airborne bacteria has been observed in areas where aerosol-producing equipment was used.1”
“Oral bacteria have been detected two meters (≈6.5 feet) from the procedure field, indicating the existence of aerosolized oral bacteria in dental practice. Aerosols can float in the air for a considerable time before being inhaled by dental staff and other patients. There is some evidence for greater prevalence of respiratory diseases and elevated antibody levels to Legionella pneumophila in dental workers.1”
1. Sawhney, A., et al. (2015). Aerosols: How Dangerous They Are in Clinical Practice. Journal of Clinical and Diagnostic Research : JCDR, 9(4), ZC52–ZC57. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437160/
_____________ is one of the greatest producers of airborne contaminants in dentistry.
Ultrasonic scaling is one of the greatest producers of airborne contaminants in dentistry, followed by air polishing, then cavity prep using a high-speed handpiece with a bur.1
“Recent studies have highlighted the spread of infection through the air resulting from the most intensive aerosol and splatter emission that occurs from an ultrasonic scaler tip and bur on a high-speed handpiece. Basu et al. surveyed aerosol-related symptoms in dental hygienists using ultrasonic scalers. They found that symptoms such as nasal irritation, persistent cough, runny eyes, and itchy and dry skin were more common in dental hygienists than in nurses and hospital staff. The coagulase-positive Staphylococcus, which was present in 6.6% of the samples, can cause a wide variety of diseases in humans through either toxin production or invasion. Of great significance, the species S. aureus is an important pathogen agent that causes wound and human skin infections and nosocomial infections. Similar results were obtained in this study confirming that the infectious airborne particles are the major risk factors for the transmission of various diseases. The control and minimization of microorganisms contained in aerosol are of great importance to the health of dental personnel. Reports have associated these aerosols with respiratory infections, ophthalmic and skin infections, tuberculosis, and hepatitis B. That research shows that both the operator and the patient are exposed to high amounts of bacteria.1”
1. Singh, A., et al. (2016). Aerosol, A Health Hazard During Ultrasonic Scaling: A Clinico-Microbiological Study. Indian Journal of Dental Research: 27(2), 160-162. Retrieved from http://www.ijdr.in/article.asp?issn=0970-9290;year=2016;volume=27;issue=2;spage=160;epage=162;aulast=Singh
Personal protection equipment (PPE) is the first layer of protection against dental aerosols. No other measures need to be taken to reduce dental aerosols or the exposure to them.
To reduce dental aerosols, and the exposure to them, clinicians should not rely on a single precautionary strategy, such as PPE alone.1
The first layer of defense against dental aerosols is to create a barrier by the donning of proper PPE, such as masks, gloves, safety glasses, and gown/lab jacket per the Occupational Safety and Health Administration (OSHA) and Centers for Disease Control and Prevention (CDC) recommendations.1
The second layer of protection is to reduce dental aerosols by the patients’ use of an antiseptic pre-procedural mouth rinse. Research shows pre-rinsing with an antiseptic mouthwash reduces bacterial recoverable colony-forming units (CFUs) by 94.1%2.
The third layer of protection in reducing dental aerosols is the routine use of a high-volume evacuator (HVE).1
“An additional fourth layer would be the use of a device to reduce aerosol contamination that escapes the operating area, such as a high-efficiency particulate air filter (HEPA). Extra-oral HVE covered with a towel can filter out blood-borne aerosols.1”
1. Paramashivaiah, R., & Prabhuji, M. L. V. (2013). Mechanized Scaling with Ultrasonics: Perils and Proactive Measures. Journal of Indian Society of Periodontology, 17(4), 423–428. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3800401/
The use of a high-volume evacuator (HVE) reduces aerosols by__________.
Research shows the use of a high-volume evacuator reduces aerosols by 90% or more when compared to an intraorally-positioned standard saliva ejector.1,2 The Centers for Disease Control and Prevention (CDC) recommend the use of high-volume air evacuation to minimize the dissemination of droplets, splatter, and aerosols.3 No preventive measure is 100% effective in reducing dental aerosols which is why dental clinicians are encouraged to use additional methods in combination (i.e., PPE, pre-procedural mouth rinse, HVE use) to reduce the number of airborne particulates produced during instrumentation.2
1. Narayana, T., Mohanty, L., Sreenath, G., & Vidhyadhari, P. (2016). Role of Preprocedural Rinse and High Volume Evacuator in Reducing Bacterial Contamination in Bioaerosols. Journal of Oral and Maxillofacial Pathology: JOMFP, 20(1), 59–65. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4860938/
2. Jacks, M.E. (2002) A Laboratory Comparison of Evacuation Devices on Aerosol Reduction. Journal of Dental Hygiene: 76(3):202-6. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12271865
3. Kohn, W.G., Collins, A.S., Cleveland, J.L., Harte, J.A., Eklunt, K.J., Malvitz, D.M. Center for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. MMWR 2003; 52 (Report No. 17). Retrieved from http://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
Which of the following has been found in aerosols produced by an ultrasonic scaler or other high-speed equipment?
Saliva, blood, gingival tissue, the nose, throat, and lungs are all sources of dental aerosols. The level of air contamination four hours after dental treatment has been found to be 3.3 times higher than before treatment.1 Tuberculosis, rhinovirus, influenza (including H1N1), herpetic viruses, and SARS have all been found in dental aerosols and can be easily transmitted to clinicians and patients.1 Those with compromised immune systems are especially vulnerable to the risk of transmission.
1. Barlean, L., et al. (2010). Airborne Microbial Contamination in Dental Practices in Iasi, Romania. OHDMBSC: 4(1), 16-20. Retrieved from https://pdfs.semanticscholar.org/c3d3/8a47d7f93e5a138522c93a0e7ae55029ee35.pdf