Do you remember the spring semester your freshman year of dental hygiene school? Filled with lingering instrumentation competencies, the anticipation of seeing your first REAL patient? As an educator, each spring when I teach polishing, students are just thrilled. They love it, and it is FUN for them! Polishing is FUN, but depending on when and where you received your education, not all polishing is treated equally. Current trends are changing the “spin” on polishing; I’d like to give you a little insight and a few tips on how to embrace the change and remember a few rules.
Abrasives are found in many dental products and have many different jobs. From sodium, potassium, and silica found in OTC toothpaste, to various grits of pumice we use chairside.
For prophy paste, the Mohs Hardness scale measures abrasiveness from 0.4-6.5, and toothpaste is measured by RDA Values. From an oral standpoint, the hardness of oral anatomy on the scale is 2-3 cementum, 3-4 dentin, and 5-6 is enamel/ apatite.
The evidence that prophy paste is a one size, one grit, one flavor, fits all kind of procedure (AKA polish all patients with coarse paste), does not hold merit3. The reason for this is we know the outer most layer of enamel is rich in fluoride, and cementum is softer than enamel. Therefore course pastes can remove and damage tooth surfaces. The current standard and ethical decision is to polish with the least abrasive paste deemed necessary by extrinsic levels, therefore, reducing the amount of tooth structure removed or potentially damaged5.
In the past, it was argued that polishing was strictly cosmetic vs. therapeutic, but is it really?
Traditionally, “selective polishing” was viewed as part of a routine prophylaxis procedure and polishing to be performed only where indicated. Back in the late 90’s, an ADHA position paper emerged, and the buzz then became polishing had negative consequences on the tooth surface and was deemed a cosmetic vs. therapeutic procedure. Selective polishing left many of us at a crossroads and patients questioning the lack of polishing.
During my undergrad work in 2007, I submitted polishing as a research topic because I taught at an institution that was very strict about polishing, and took heed to the ADHA position paper. To my surprise, there was very little clinical evidence one way or the other. However, what did emerge around this time was different products, with a variety of ingredients, to aid in therapeutic value.
Since then, we have seen a therapeutic trend in polishing pastes, and the term therapeutic has evolved. Not much has changed in textbooks or journals about the rule for choosing the correct grit prophy paste, we know that when polishing is indicated using the least abrasive paste is still the rule of thumb, however, we now find that multiple paste options are available to help with such choices.
As research emerged on fluoride, calcium, and remineralization, manufacturers jumped on the bandwagon and began modifying their pastes. What we see on the market now, are additives and ingredients in prophy pastes that DO make them therapeutic with the delivery of medicaments to the tooth surface. For instance, what’s inside today’s smart pastes is not only a range of abrasive grit formulas, but other active ingredients such as fluoride, ACP, CPP, NovaMin, xylitol, and arginine bicarbonate5.
These pastes are a topical delivery method providing therapeutic benefits for caries, sensitivity, and remineralization. We even see such smart pastes that are packaged with two varied grits to aid in more selective polishing. When I teach selective polishing as a means to remove stain, and provide additional therapy, it is imperative that clinicians choose a paste that meets the patient’s clinical needs. No longer is polishing just cosmetic, or about the removal of biofilm alone. It can provide both therapeutic and motivational benefits which is win-win!
Let’s touch briefly on air polishing. Traditionally sodium bicarbonate or aluminum trihydroxide powder is used under pressure to aid in extrinsic stain removal. Performed properly it is fast, efficient, and less fatiguing for the clinician3,5. This powder is less abrasive overall, but references still recommend that areas of cementum restorations be avoided. The downside is that this powerful biofilm blaster is a bit technique sensitive and requires the clinician to be savvy to control the water, powder, and patient comfort. Let’s face it, not all hygienists enjoy the use of an air polisher due to it messy nature
When to polish?
One topic of debate is when to polish? As research emerged and the focus on biofilm removal became our focus (vs. solely calculus removal), now is a good time to remember ultrasonic technology can disrupt biofilm. Today, we see an increase in the use of ultrasonic debridement. Some hygienists prefer to polish/air polish to remove heavy supra biofilm before scaling. There is a lot of variation to be had, but the bottom line questions still exist; polish, don’t polish, polish before or after scaling?
What if the future holds the best of both worlds and we could obtain a way to remove and reduce biofilm without harming the dentin or cementum while providing therapeutic value to our patients? What if it were quick and efficient? I say ride the wave! Here is how…
Now, if you are a seasoned hygienist, this may ruffle your feathers a bit, but I can assure you I have also had to embrace change and allow for innovative thinking. For me, only by doing is seeing and believing. I am certain the wave of the future will lay in glycine therapy. Today’s RDH recently published an article with specifics to glycine biofilm removal and its’ benefits2. There is research going back to 2008 supporting the role of biofilm removal regarding peri-implantitis.
I have been fortunate to represent ACTEON, as a clinical products trainer, over the past few years. I have been able to put this technology to work for me and help others implement it in their practices. I am a firm believer that the benefits of using glycine will truly be in the best interest of our patients. What I see most often in offices, and with talking to other hygienists, is apprehension to change. Change means something different and usually takes time, but it is achievable, and as professionals, ethically we must remain current with evidence-based protocols.
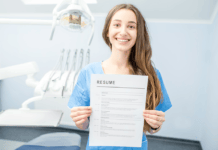
I want to encourage you to embrace this upcoming technology and give you a few tips on how and where to start! Here are three steps to successfully implementing glycine polishing in your practice:
- Educate yourself, your Doctor, and hygiene team, to embrace this technology. (check out Acteon and Hu-Friedy for the latest equipment)
- Inquire and schedule a session with a representative to make an informed decision.
- Set a date to have the clinical trainer come immediately when the equipment arrives, and again after 2-3 weeks.
My secret to success is after your training session, disconnect your slow-speed handpiece and put it away for two weeks straight! It is tempting to return to what is comfortable, and tempting to pick up your handpiece in a pinch. My goal for hygienists is to be comfortable, confident, and efficient with air polishing equipment. If you give it about two weeks, you will wonder how you lived without it!
Embracing technology, and advances we see in dental hygiene, means we are treating patients and their disease with intent. The standard one size, one prophy fits all is a way of the past. The future in dental hygiene is linked to oral health and systemic health and targeting biofilm, inflammation, and chronic disease. Selective polishing still has its place in the operatory, but I hope I have opened your eyes to a new and improved technology that will do more than put a sparkle in your smile!
SEE ALSO: Ask Kara RDH: Only Polishing Children & Considering it a Prophy
DON’T MISS: FREE CE: Coronal Polishing Webinar – Take a Spin In a New Direction
Now Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- (2018) Retrieved from https://www.acteongroup.com/en/my-products/equipment/airpolisher/air-n-go-easy
- Carmen L. (2018) Air Polishing: We’ve come a long way baby. Today’s RDH, March 18, 2018. Retrieved from https://www.todaysrdh.com/air-polishing-weve-come-a-long-way-baby/
- Darby, M. & Walsh, M. (2014). Dental Hygiene Practice and Theory, 4th Ed https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4555792/
- (2018) Airflow Therapy. Retrieved from https://www.hu-friedy.com/BIOFILM
- Wilkins, E. (2017). The Clinical Practice of Dental Hygiene, 12ed.