According to the Alzheimer’s Association, Alzheimer’s disease is the 6th leading cause of death in the United States, with someone in America developing the disease every 65 seconds. Periodontal disease attacks approximately half of United States adults over age 30, with prevalence rates rising to around 70% in adults 65 and older. When we look at the stats on Alzheimer’s and periodontal disease, it’s clear both present troubling rates of incidence in the United States, particularly for older adults.
But what do these two diseases have to do with each other? Although periodontitis has long been considered a risk factor for Alzheimer’s, recent research from the University of Illinois at Chicago shows strong evidence that Alzheimer’s might be kickstarted in the body by the bacteria associated with periodontal disease.
What causes Alzheimer’s?
Researchers have struggled to pinpoint the cause of this debilitating form of dementia which creates issues with memory, thinking, and behavior. Thought to be caused by a complex combination of genetic factors, age, and heart health, Alzheimer’s is associated with abnormalities in the brain, including plaques and tangles which prevent adequate communication between nerve cells. It’s associated with a protein called beta amyloid, that creates the damaging plaques which prevent neurons from communicating. It’s associated with greater inflammation and neurodegenerative effects.
According to the University of Illinois at Chicago research team, the type of brain dysfunction associated with Alzheimer’s is also seen with the introduction of periodontal bacteria in mice models. This highlights the link between the two—and provides a fascinating area open to further research in both diseases and their relationship.
The Study
In this recent study, researchers found some fascinating changes in the brains of mice exposed to periodontitis. Researchers induced chronic periodontitis in ten eight-week-old mice for 22 weeks. Afterward, researchers collected brain tissue from the mice who had been exposed to periodontal bacteria and made the following discoveries:
Pg/gingipain: mouth to brain
Pg/gingipain bacteria was found in the brain tissue of infected mice. This showed that the periodontal bacteria had indeed traveled from the mouth to the brain tissue of infected mice.
Microgliosis and astrogliosis
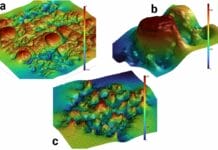
Researchers found microgliosis and astrogliosis in the experimental group and not the control group. Microgliosis refers to an increasing number of microglial cells, which is known to have a pro-inflammatory effect in the brain. Astrogliosis refers to an increasing number of astrocytes, which are associated with infection. This was notable due to the similar inflammatory effects observed in brain tissue with Alzheimer’s disease.
Neurodegeneration
The effects of neurodegeneration were found in the experimental group. In Alzheimer’s disease, the hippocampus is the part of the brain which shows symptoms of degeneration. In the study, the brain tissue of infected mice showed three pro-inflammatory cytokines that didn’t appear in the brain tissue of the control group.
Fewer neuronal cells
The researchers knew inflammation in the brain generally damages neurons, and they tested this during this study. The results? The control group had a greater density of neuronal cells. The experimental group showed a “statistically significant” decrease in neuronal cell density, which is a hallmark of a brain with Alzheimer’s.
Increased proteins in brain tissue
Proteins like phospho-tau and beta amyloid were found in a greater degree in the brain tissue of mice which had been subjected to periodontal bacteria. Accumulation of these proteins is linked to diseases like Alzheimer’s because it contributes to the plaques that block neurons from communicating.
Periodontitis & Alzheimer’s
At the study’s end, researchers felt confident stating periodontal bacteria can initiate neurodegenerative effects in mice after only 22 weeks of infection. The type of neurodegenerative effects they noted was consistent with findings in the brains of people who are diagnosed with Alzheimer’s Disease.
This research presents a fascinating development in research regarding difficult-to-treat Alzheimer’s disease. Especially considering periodontal disease is controllable and treatable, this latest research presents a fascinating and hopeful glimpse into supporting neural health through managing periodontitis. Though there are abundant reasons to take special care with oral health, this study highlights the importance of supporting overall health through managed oral care.