We’ve long known that there was a correlation between chronic health risks, such as arthritis and diabetes, and periodontal disease rates; however, the reasons why have always eluded researchers. But a team of University of Toronto researchers may have finally established the missing link, and their study published in the Journal of Dental Research reveals it’s all due to your body’s natural responses to inflammation.
Explaining the Link Between Systemic Health and Dental Health
In a systematic review of more than 1,200 different research reports, the U.S. Centers for Disease Control and Prevention found strong associations between periodontitis, dental caries, and tooth loss with numerous chronic systemic diseases, including:
- Diabetes
- Cardiovascular disease
- COPD
- Dementia
- Psoriasis
- Lung cancer
- Cerebrovascular diseases (i.e., stroke, etc.)
While there is a link across the board, some specific dental conditions have stronger associations with specific systemic health problems. For example, there’s a strong association between periodontitis and diabetes and between tooth loss and cerebrovascular disease.
And although thousands of studies have already supported this link between systemic disease and dental disease, the underlying mechanism was still unclear as recently as 2019. Thus, the new research from the dental faculty at the University of Toronto is truly groundbreaking.
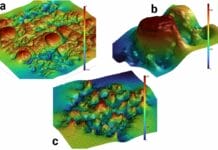
In this study, released in October 2020, the researchers analyzed the activity of neutrophils.
Neutrophils are a type of white blood cell in the immune system that responds to infection and releases various enzymes designed to kill microorganisms in your body.
The study noted that in the case of periodontal disease, the body naturally releases these immune system cells to attack the bacteria responsible for periodontal disease. And while this activation of the immune system is necessary for handling periodontal disease, these neutrophils’ activity was not restricted solely to the tissues in and around the mouth. Instead, the neutrophils circulated throughout the entire body and, in some cases, responded to secondary infections found in the body.
It’s this secondary response that the researchers identified as being connected to an increase of other systemic diseases. As the white blood cells do their work, they release inflammatory compounds and damage other cells and tissues in the body, playing a role in developing other illnesses and diseases.
To put it simply, when someone develops periodontal disease, the body sends neutrophils to combat the bacteria in and around the teeth and gingiva. But the neutrophils spread throughout the entire body, overreacting and damaging other cells in the body, leading to an increase in other systemic health problems that we’ve long seen in thousands of research studies.
What This Research Suggests for Dental Hygiene
This study answers the underlying association between dental health and a patient’s overall health. And it further supports the critical importance of dental hygiene, not just for oral health but also for the reduction of heart disease, stroke, diabetes, and more.
Dental hygienists and dentists need to educate their patients on this important link and emphasize the importance of regular exams and preventive dental hygiene care.
In a press release discussing the study, the University of Toronto also underscores the importance of this study as it relates to dental hygiene and current health concerns worrying society.
By helping patients to think about the big picture, hygienists can advocate for their patients’ health and motivate patients to seriously consider how their dental hygiene affects any other health worries that they may have.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below: