Dental hygienists are likely to encounter individuals who are living with serious mental illness, including people who may be at risk for suicide.1 Medical history and verbal disclosures shared with dental hygienists may include details about antipsychotic and antidepressant medications or symptoms and a history of mental illness and/or substance use, including tobacco.
Friends, family, and the healthcare team need the knowledge, skills, and ability to support and care for individuals impacted by mental health conditions. Many people experience mental health conditions, including psychosis, other emotional and mental health conditions, and substance use. One in five people in the United States experiences a mental health condition at some point in their lives.1
Prevention Strategies
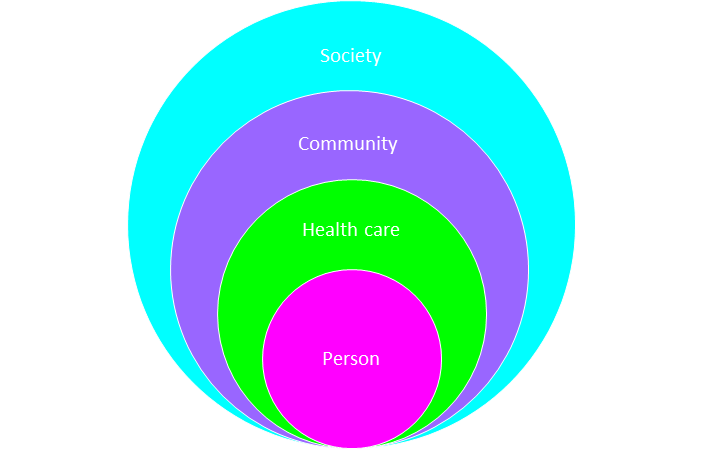
Societal level and community level resources ─ There are courses available to further your skills related to mental health and suicide prevention. A highly recommended program is Mental Health First Aid from the National Council for Mental Wellbeing. Mental Health First Aid teaches skills to help the people in your life get to care when and if they need mental health care.
Mental Health First Aid is available to everyone, and there is a teen version, too. Training is available throughout the United States; it would be great for dental hygienists to learn from this program. To find a training, visit www.MentalHealthFirstAid.org.3
Additional courses are available, especially for caregivers (people with loved ones who struggle with mental health conditions). One such training is QPR, which stands for Question, Persuade, and Refer – three simple steps that anyone can learn to help save a life from suicide. Just as people trained in CPR and the Heimlich maneuver help save thousands of lives each year, people trained in QPR learn how to recognize the warning signs of a suicide crisis and how to question, persuade, and refer someone to help.4
Another way to learn to support individuals is an intensive program that mental health professionals and caregivers use called ASIST. LivingWorks’ ASIST has been “empowering people to provide skilled, lifesaving interventions for over 35 years.”5 A shorter training is LivingWorks’ SafeTALK, which promotes learning “powerful, lifesaving skills in just four hours.” 6
The MANDT System is training in de-escalation with verbal and physical tactics, recommended for providers working closely with special populations. De-escalation prevents escalating individuals into crisis. To sign up or find resources, visit Mandt.7
If you’re looking to learn from engaging information, peer support can be found online by searching #mentalhealth on social media, #mentalhealth in podcasts, and by linking to your local library to request reading lists of mental health themes.
Interpersonal Listening Skills for the Dental Team
Dental hygienists need skills to listen when mental health or substance use conditions are disclosed. If a hygienist can see an individual’s strengths, the hygienist can see their humanity. When providers or others lack social skills to accept the listener role, patients may feel stigma. Stigma happens when the listener receiving the information reacts with negative nonverbal and verbal cues. It may stem from listeners who rely on negative stereotypes, which may lead to discrimination.8
Try to stay in connection and try to avoid disconnection. Examples of positive nonverbal and verbal cues include maintaining distance, relaxed posture, and saying thoughtful replies.
Dental hygienists often have the skills necessary to support individuals in recovery from mental health and substance use. Listening skills and validating feelings may help patients. Being able to see the person’s characteristics such as strength, bravery, humor, and thoughtfulness. Other characteristics such as the ability to address their dental needs by attending the appointment may help reduce stigma.
Provider awareness and acknowledgment of the concept of resiliency and mental health recovery and/or substance use recovery is important.
If you are concerned about an individual’s mental health and substance use (including tobacco use), then recommend referral. Referrals include primary care and a behavioral health care provider. For mental health medication, patients will need a mental health prescriber, but also addressing any underlying health conditions is essential to overall health and wellness. Prescription and over-the-counter options help with quitting tobacco. Screening, brief intervention, and referral to treatment (SBIRT) are ideal for use in a dental practice, including pediatric patients.9
Suicide Screening and the Dental Practice
There is little research or knowledge related to screening for suicide as a part of dental care. Some hospital systems mandate a brief screening called ASQ (Ask Screening-Suicide Questions) for all pediatric patients to reduce the incidence of the child suicide epidemic, including specialty clinics (dental specialty clinics are included).10,13 Schools (while not required to document the use of the suicide protocol) use the protocols in children as young as preschool.
Suicide is often overlooked in young children ages five to 10. According to the American Psychological Association (APA) though, suicide is the third leading cause of death in this age group.11
Dental providers’ Collaboration with the Medical and Mental Health Teams
Oral care is a health behavior and may be an early warning sign or indicator of a change in health status. If there is a drastic change in oral health status due to a change in an activity of daily living, this could indicate a change in mental health status. Tooth brushing and interdental cleaning are activities of daily living that may be considered part of self-care. Mental illness may be associated with a change in functional ability, especially when individuals experience psychiatric disability. Referral for assessment of underlying mental health conditions is an important issue, especially for youth.
In addition, brief motivational interviewing may be effective for oral health behavior change.12 Working with the therapist may be important as a part of whole-person health care, especially when patients have experienced trauma.
Collaboration with therapists can enhance the quality of patient care. Integrated oral and behavioral health care is well described in a 2020 presentation by the National Council for Mental Wellness, Center of Excellence for Integrated Health Solutions.13 If a patient has special dental needs, including anxiety or other mental health conditions, it may enhance care to reach out to licensed mental health providers (therapists and psychologists).
An informed approach is to ask patients on medical histories prior to office visits if they have any wishes for you to collaborate with their mental health care team to improve oral health care experiences (especially if dental anxiety is indicated on their health history). Outreaching to the therapist before the appointment is best.
If you have a procedure manual in your office, you can share your written protocols for patient care. This can help prepare patients for oral care interventions they may need. Therapists can help support patients coping with fears and trauma. Ask the mental health provider how best to support your patient during care, and if there are any particular “triggers” or stimulus to avoid that you should be aware of.
Role of Medications
Since 1952 when chlorpromazine was introduced, mental health care has evolved over the past 69 years.14 Some 50 antipsychotic medications have been marketed in the United States, and these medications may reduce symptoms of psychosis.14
The deinstitutionalization of psychiatric patients began in the 1970s and 1980s. From the advent of antidepressants in the 1990s to the criminalization of mental illness in the past 50 years, we stopped treating severe mental illness separately as a population.
There are significant impacts of mental health care treatments on oral health, and there may be serious side effects. There are five primary medication types in mental health conditions, and the common side effect is xerostomia.
- Anxiety medication
- Stimulants (ADHD)
- Antidepressants
- Antipsychotics
- Mood Stabilizers
Trauma and Resiliency
Trauma can increase the risk of severe mental illness, and much work has been done through the work of the adverse childhood experiences screenings (ACES) to help identify and link the score to diseases.15 However, protective factors and early access to care resiliency and recovery are a reality for many. For more information about trauma-informed primary care, visit: https://www.thenationalcouncil.org/fostering-resilience-and-recovery-a-change-package/
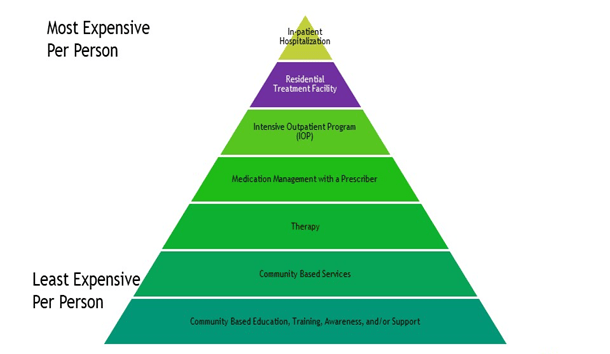
Mental health care services ─ A client handbook may help orient individuals to the care system.16 For most individuals who are not in crisis and who plan to access care in a fee-for-service private health system, medication management with a prescriber is usually the first step in the medical model of care delivery (see Figure 2). A mental health prescriber such as a psychiatrist, psychiatric nurse practitioner, or medical doctor is usually the first step in accessing care.
A referral to a therapist may be warranted in alternative scenarios when medication isn’t necessary or to supplement a medication’s effectiveness. For some individuals, a counselor may be a resource. A licensed master social worker (LMSW) or a psychologist provides mental health treatment commonly referred to as therapy. Some individuals are certified peer support specialists who can provide support during a recovery journey, and certified peer mentors work with substance use recovery.
Together, a mental health team may help individuals in recovery, but ultimately the journey belongs to the patient. When experiencing mental illness, it can be challenging to determine the best course of treatment and decide how best to manage diseases that may complicate mental health. There are resources if you or a loved one are in crisis, especially resources from groups like the National Alliance on Mental Illness and their guide to navigating a mental health crisis which is available online.17
If an individual cannot access care early and waits until a mental health crisis, sometimes events escalate and result in the need for a mental health emergency response with a 9-8-8 call (starting in July 2022), which will be the national number for a mental health crisis.18 There is family de-escalation training called Family Mandt that focuses on both verbal and physical de-escalation techniques available in the community.
A crisis intervention team (CIT) (trained law enforcement officer and a co-responder, a licensed mental health provider) are individuals who visit a house when there is a call about a mental health crisis. If indicated, hospitalization followed by intensive outpatient programs, including medications management with a prescriber, therapy, and other education and community supports, can benefit individuals.
If a person is a threat to themselves or others, 9-1-1 is recommended, and be sure to share it is a mental health emergency, so the operator knows to engage specially trained law enforcement officers and a co-responder.
Person level ─ There are healthy activities that can benefit well-being. This list originates from Maslow’s hierarchy of needs, medical necessity, and avoiding substance use.19-21
- Self-care may include things that help restore your spirit. Activities such as taking a long bath, oral care, doing yoga, writing, your favorite exercise routine, or even performing standup comedy can be restorative.
- Coping skills are your ability to get your needs met, including communication skills and activities to keep you safe. Resources include mindfulness, meditation, phone apps, community resources, gratitude, journaling, mindful breathing, creating a self-care plan, identifying healthy supports, and a focus on hope for recovery.
- A stable living environment can contribute to mental wellness.
- Attending work, school, and activities may benefit wellness or indicate that you’re coping and well.
- Nutrition is one of the most important factors for well-being.
- Sleep is essential to mental health and well-being.
- Medication adherence (if needed) may be an essential factor for well-being.
- Avoiding tobacco use may make medication and overall health and well-being better.
- Avoiding substance use is essential to overall health and well-being.
If these items don’t help and you’re experiencing mental health symptoms, please recommend seeking professional mental and healthcare services.
There is hope with treatment. Recovery is possible. Hope and courage are two critical ingredients in healing from mental illness or substance use.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Navigating a Mental Health Crisis. (2018). National Alliance on Mental Illness. Retrieved from https://www.nami.org/Support-Education/Publications-Reports/Guides/Navigating-a-Mental-Health-Crisis/Navigating-A-Mental-Health-Crisis
- Golden, S.D., Earp, J.A. Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions. Health Educ Behav. 2012; 39(3): 364-372. doi:10.1177/1090198111418634.
- Mental Health First Aid. https://www.thenationalcouncil.org/about/mental-health-first-aid/
- Question. Persuade. Refer. (QPR). The Speedy Foundation. Retrieved from https://www.thespeedyfoundation.org/qpr
- LivingWorks Assist. Living Works. Retrieved from https://www.livingworks.net/asist
- SafeTALK. Living Works. Retrieved from https://www.livingworks.net/safetalk
- The Mandt System. Retrieved from https://www.mandtsystem.com/
- Mental Health: Overcoming the Stigma of Mental Illness. (2017, May 24). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health/art-20046477
- Cuevas, J., Chi, D.L. SBIRT-Based Interventions to Improve Pediatric Oral Health Behaviors and Outcomes: Considerations for Future Behavioral SBIRT Interventions in Dentistry. Curr Oral Health Rep. 2016; 3(3): 187-192. doi:10.1007/s40496-016-0106-y.
- Ask Suicide-screening Questions Toolkit. (n.d.). National Institute of Mental Health. Retrieved from https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/index.shtml
- Weir, K. Research on Suicide Overlooks Young Children; Psychologists Are Working to Change That. American Psychological Association. 2016; 47(11): 28. Retrieved from https://www.apa.org/monitor/2016/12/ce-corner
- Wide, U., Hagman, J., Werner, H., Hakeberg, M. Can a Brief Psychological Intervention Improve Oral Health Behaviour? A Randomised Controlled Trial. BMC Oral Health. 2018; 18(1): 163. doi:10.1186/s12903-018-0627-y. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6171315/
- National Council on Mental Wellness. Center of Excellence for Integrated Health Solutions. (2020, August 19). Retrieved from Oral Health & Behavioral Health: Models of Coordinated and Integrated Care – Zoom
- Li, M. Antipsychotic-induced Sensitization and Tolerance: Behavioral Characteristics, Developmental Impacts, and Neurobiological Mechanisms. J Psychopharmacol. 2016; 30(8): 749-770. doi:10.1177/0269881116654697.
- Hughes, K., Bellis, M.A., Hardcastle, K.A., et al. The Effect of Multiple Adverse Childhood Experiences on Health: A Systematic Review and Meta-analysis. Lancet Public Health. 2017; 2(8): e356-e366. doi:10.1016/S2468-2667(17)30118-4.
- Johnson County Mental Health Center Client Handbook. (2021). Johnson County Mental Health Center. Retrieved from https://www.jocogov.org/sites/default/files/documents/MNH/jcmhc_client_handbook_final_2021.pdf
- Brister, T. (2018). Navigating a Mental Health Crisis. NAMI. Retrieved from https://www.nami.org/Support-Education/Publications-Reports/Guides/Navigating-a-Mental-Health-Crisis/Navigating-A-Mental-Health-Crisis
- Sparling, Z. (2021, January 30). Oregon Gets Grant for 988 Suicide Prevention Hotline. Portland Tribune. Retrieved from https://pamplinmedia.com/pt/9-news/496397-398244-oregon-gets-grant-for-988-suicide-prevention-hotline
- Eggerth, D.E., Flynn, M.A. Applying the Theory of Work Adjustment to Latino Immigrant Workers: An Exploratory Study. J Career Dev. 2012; 39(1): 76-68. doi:10.1177/0894845311417129.
- Nieuwlaat, R., Wilczynski, N., Navarro, T., et al. Interventions for Enhancing Medication Adherence. Cochrane Database Syst Rev. 2014; 2014(11): CD000011. doi:10.1002/14651858.CD000011.pub4.
- Screening, Brief Intervention, and Referral to Treatment (SBIRT). (2017, September 15). Substance Abuse and Mental Health Service Agency. Retrieved from https://www.samhsa.gov/sbirt











