Scientists have made a recent discovery that could impact patients diagnosed with osteoporosis. The findings from the study were published in the FASEB Journal by the Federation of American Societies for Experimental Biology under the title “Laser irradiation decreases sclerostin expression in bone and osteogenic cells.” Researchers hope dentists may be able to use laser irradiation as a potential treatment for patients with osteoporosis in need of periodontal surgery due to its beneficial therapeutic effects and biological responses.
Information About Osteoporosis
According to the National Osteoporosis Foundation, over 54 million Americans are living with osteoporosis. The disease, which means “porous bone,” occurs when someone suffers from the loss of bone mass, and it becomes weak over time. As a result, patients diagnosed with osteoporosis are more likely to experience bone fractures in their hip, spine, and wrist as a result of their brittle bones.
There are certain risk factors that can make someone more susceptible to being diagnosed with osteoporosis. For example, non-Hispanic, white, and Asian women have a higher chance of developing osteoporosis than women from other ethnic backgrounds. Research also shows that people over the age of 50 are more at risk. Certain medications, diseases, and medical procedures can also increase the chances of developing osteoporosis as they age.
The National Institute of Health recommends that patients with osteoporosis consult their dentists and other medical professionals, so they can take that into consideration when developing a treatment plan. Factors that can prevent or decrease the chance of bone loss include exercise, certain medications, proper nutrition, lifestyle changes, and using devices to prevent indoor falls.
About the Study
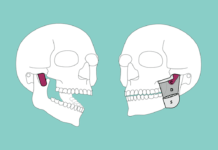
Periodontists use lasers during periodontal surgery as an effective way to heal tissue and regenerate bones. A team of researchers at Tokyo Medical and Dental University (TMDU), led by Yujin Ohsugi, noticed that patients healed faster with Er:YAG lasers than when they underwent periodontal surgery with bur drilling and decided to investigate why.
After much deliberation, the scientists decided to examine whether laser irradiation interfered with Sclerostin expression, a glycoprotein coded by the SOST gene in the bone. Sclerostin is produced by bone cells, suppresses bone formation, and plays an important role in bone remodeling, where mature bone tissue is removed from the skeleton, and new bone tissue is formed.
To conduct the study, Ohsugi and the other researchers compared and contrasted the biological healing responses of laser-ablated, bur drilled, and untreated bone on rat skull bones. They examined how Er:YAG laser irradiation affected osteogenic cells and sequential gene expression. Using microarray analysis, they closely examined the gene expression patterns exhibited by the rat skull bones during a 6, 24, and 72 hour time period after they underwent drilling or laser treatment. The researchers performed an immunohistochemical analysis after 24 hours to detect the glycoprotein Sclerostin. The scientists also closely studied their sample of osteogenic cell cultures for evidence of sclerostin expression and dying cells. The microarray analysis displayed a clear distinction in the gene expression pattern between laser-ablated and bur-drilled rat skull bones after only 24 hours.
Ohsugi revealed the researchers were able to find both in vivo and in vitro evidence that the mechanical stimulation of Er:YAG laser irradiation decreases the level of sclerostin expression in bone and osteogenic cells. Besides inhibiting sclerostin, the Japanese team also discovered that the laser-based therapeutic treatment does not cause inflammation to develop, unlike the more conventional bur-drilling technique.
Ohsugi believes laser irradiation shows promise as a new treatment modality for dental patients with osteoporosis since it does not provoke inflammation. Overall, their findings may help advance research towards the development of laser-based therapeutic methods that can improve bone regrowth during periodontal and orthopedic surgery.