Have you ever thought about treatment acceptance and the feeling of a “yes” from a patient? It’s probably one of the most exciting moments of a dental appointment. The sweet moment is when a patient accepts your expert clinical suggestion for their dental health and agrees to a set standard of care.
Don’t get me wrong, it’s not like we are looking to upsell treatment or sell a particular product. Rather, it’s more about establishing an understanding of the treatment being proposed. It’s about developing a level of respect from the patient for the care received. With more information, the patient can make a sound decision.
What do I mean by proposed? Well, it simply means an individual needs-based treatment plan is constructed that aligns with the patient’s oral health needs and has a set timeline for optimal benefits for the patient.
Suggesting “Areas of Concern” as a Secondary Voice for the Dentist
This approach doesn’t just limit us to our dental hygiene diagnosis and treatment options. This can also include dental work that may benefit the patient’s periodontium and overall oral health, such as overhang correction or flap surgery.
For you as a clinician to be able to suggest “areas of concern” during a recare or non-surgical periodontal therapy appointment, it’s important to be informed on all the procedures that the dentist can perform and typically recommends. Having a professional relationship with referring doctors who provide care to your patients is also a great idea. Staying informed on procedures and referring practices enables you to present treatment comfortably and confidently as a hygienist.
You may possibly provide the patient with examples of the dentist’s work or details on treatment options, duration of appointments, or sequence of treatment. Simultaneously, it’s important always to reiterate that the dentist will have to diagnose after a thorough assessment. By verbalizing this to the patient, you are ensuring the patient understands that you are not making a diagnosis and simply providing a suggestion based on your clinical expertise and experience. Together with your and the dentists’ findings, you can curate a diagnosis with a treatment plan proposal for the patient.
Don’t hesitate to be the secondary voice for your dentist. You are working alongside the dentist as a counterpart. As a clinician, there is an ethical standard and expectation on your part to keep the patient informed of their oral status.
Coordinating the Flow of Information
Having discussions chairside about patients’ needs allows them to process the potential care suggested prior to the dentist providing their examination. It’s often noted that patients typically wait until after the dentist exits the operatory to ask more questions about any treatment that may have been proposed. This tends to come from a lack of full understanding or merely not processing the diagnosis quickly enough.
Patients also report not understanding the treatment correctly or the diagnosis being vague in explanation. Unfortunately, this can take away from chair time if it’s during the latter half of the appointment. The patient may probe you for more information regarding the diagnosis, possibly causing you to run late for the next appointment. On the other hand, in some cases, this can also lead to you rushing through answering important patient questions regarding treatment, resulting in declined or postponed treatment.
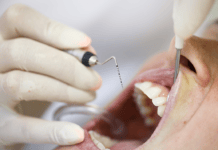
This is where knowledge is power. You want to provide information directly and concisely. Don’t just speak to the patient through thin air. Show them examples, whether in the form of a video, photo, radiograph, or typodont.
I’ll say it repeatedly: Take that intraoral photo! It will be the most powerful tool during the appointment and presentation process. The ability for a patient to visually see what is happening in their mouth can be a huge turning point for many.
It can also be a great trigger point for open-ended questions. As clinicians, we want to encourage patient involvement. A lack of understanding is the most common reason patients decline proposed treatment plans. We’ve all seen or experienced a rushed appointment that later results in the dismissal of the proposed treatment.
In Closing
To sum up, we all understand that, as dental hygienists in most states and Canadian provinces, we are not able to diagnose. However, we are able to suggest “areas of concern” and pre-screen prior to the doctor’s examination.
During your allocated time with the patient, take note of all areas that may require attention. This will be translated to the dentist and, in turn, will be reflective of your detailed care. Engage in conversation that will educate the patient on their current oral status while bringing concerns and areas of risk to light. Use all the tools available to you in the practice to educate the patient.
Not only is this important when presenting care proposed by the dentist but also when presenting care under your scope of practice. This will result in higher acceptance rates, a successful practice, and healthier patients.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.