An understanding of the mechanism, the purpose, and dosage will help determine when and why multiple blood pressure medications are used. Simple lifestyle changes (such as diet, exercise, and weight loss) can lower blood pressure. When blood pressure is very high, and lifestyle measures have failed, medications are commonly prescribed.
Some blood pressure medications work in the heart. Others work in the blood vessels and some control fluid retention. Most hypertensive medications have multiple uses for the treatment of different medical conditions. This article concentrates on the effects of medications on hypertension.
Dental professionals should have an understanding of blood pressure medications because many may cause oral side effects and dental treatment implications. A few oral side effects of common hypertension medications, dependent on each medication, include altered taste, numbing of the lips and mouth, xerostomia, and gingival hyperplasia. Dental treatment implications dependent on certain medications may consist of postural hypotension, slowing the metabolism of lidocaine, bupivacaine, and mepivacaine, and the vasodilatory inhibition effect of epinephrine. Further, dependent on the medication, epinephrine may cause tachycardia.
High Blood Pressure
High blood pressure, also called hypertension, is when the force of blood pushing against the blood vessels’ walls is consistently too high. As the heart beats, it creates pressure that pushes blood through a network of vessels, including arteries, veins, and capillaries. The more the heart pumps and the narrower the arteries become, the higher the blood pressure.
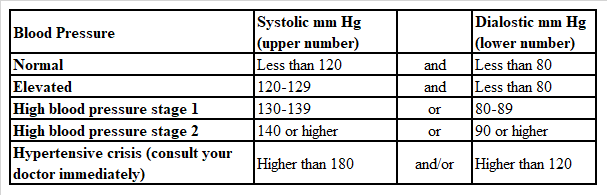
This pressure is the result of two forces − systolic and diastolic. Systolic pressure occurs as blood pumps out of the heart and into the arteries and is part of the circulatory system. The diastolic pressure is created as the heart rests between heartbeats. These two forces are represented in numbers1 (see Figure 1).
Blood Pressure Causes
Causes of high blood pressure are primary and secondary. Primary is when it develops gradually over the years and without any distinct cause. Secondary is developed by underlying conditions and appears suddenly and tends to cause higher blood pressure than primary. Various conditions are obstructive sleep apnea, kidney disease, adrenal gland tumors, thyroid problems, congenital blood vessel defects, medications, and illegal recreational drugs.2
The risk factors for high blood pressure include:
- Age. Higher in men until about age 64, women are more likely to develop high blood pressure after age 65.
- Race. More common in African Americans and develop at a younger age.
- Family history.
- Overweight or obesity. More weight requires more blood to supply oxygen and nutrients to the tissue. With more blood flow through the vessels, the more pressure is put on the arteries.
- Lack of activity. Inactivity causes higher heart rates. This increases the workload of the heart, and with each contraction, it provides more force on the arteries.
- Tobacco use. Smoking and chewing tobacco spontaneously raise blood pressure temporarily. The chemicals in tobacco also cause damage to the lining of the artery walls.
- Too much sodium. Excessive sodium can cause fluid retention.
- Too little potassium. If the body lacks potassium, it can cause sodium to build up in the body.
- Alcohol. Heavy drinking can damage the heart.
- Stress. High levels can lead to a temporary increase in blood pressure.2

Review of Medications
Diuretics: Diuretics, also known as water pills, increase urination to remove the excess sodium and water from the body to lower blood pressure. Several classes of diuretics work in distinct ways and in different parts of the kidney. They are often used in combination with other medications. While diuretics are used in sole therapeutic agents for high blood pressure, there are also other uses for them.3,4
Other uses: In adjunct therapy for edema associated with congestive heart failure, cirrhosis of the liver, corticosteroid, and estrogen therapy.4
Carbonic anhydrase inhibitors: Carbonic anhydrase inhibitors are used mainly in the treatment of glaucoma by reducing fluid levels in the eye and are used as off-label altitude sickness. They act by excreting the increase of bicarbonate, sodium, potassium, and water from the kidneys. These are weak diuretics.
Other uses: Chronic simple (open angle) glaucoma and secondary glaucoma.
- Acetazolamide (Diamox): Initial dose 125 mg. Maintenance dose 250 mg. Maximum dose 500 mg.
Side effects: Drowsiness and confusion; hearing problems (tinnitus); nausea, vomiting, loss of appetite, diarrhea; numbness or tingling in the arms and legs.
Drug interactions and precautions: Metformin, Topamax, Xanax, Cymbalta, aspirin, and prednisone.5
Dental concerns: Altered sense of taste, numbing of lips and mouth.
Thiazide diuretics: Thiazide diuretics inhibit the sodium/chloride cotransporter in the distal convoluted tubule of a kidney cell. This decreases the amount of sodium reabsorbed back into the body, which results in more fluid being passed as urine. They also widen blood vessels, causing lowered blood pressure.
Thiazide diuretics are used for high blood pressure when the body accumulates too many fluids such as with heart failure. Thiazides have a weak action on the kidney, so there isn’t a great increase in urine, and that is why they are considered relatively weak diuretics. Thiazides will tend to end in –thiozide.4
Other uses: Although non-FDA approved, they are used for osteoporosis in postmenopausal women, used in conjunction with calcium or estrogen, and treating diabetes insipidus.6
- Chlorthalidone (Thalitone): Initial dose 25 mg once a day. Maintenance 25 to 100 mg. Usual range 12.5-25 mg. Maximum range 100 mg once a day.
- Chlorothiazide (Diuril): Initial dose 500 to 1000 mg once a day or divided dose. Maximum 2000 mg. a day in divided doses.
- Hydrochlorothiazide HCTZ (Aquazide H, Microzide): Initial dose 25 mg once a day. Maintenance dose 50 mg once a day or in divided doses. No more than 50 mg is usually needed when other blood pressure medications are used.
- Indapamide (Lozol): Initial dose 1.5 mg once a day in the morning; if not responsive after four weeks, increasing dose to 2.5 mg once a day; and if not responsive after another four weeks, increase dose to 5 mg once a day and adding another blood pressure medication for therapy.
- Metolazone (Mykrox, Zaroxolyn): Initial dose 2.5 mg once a day. May be increased to 20 mg once a day.4
Side effects are uncommon as these diuretics are low doses for lowering blood pressure. But side effects may include: increase in blood pressure; increase in uric acid causing gout attacks; a salt imbalance that causes low blood level of calcium, sodium, and magnesium, which can cause weakness, confusion, and abnormal heart rhythms; upset stomach, skin sensitivity to sunlight, and impotence (reversible when medication is stopped).
Drug interactions and precautions for thiazide diuretics: Lithium, digoxin, NSAIDs, dofetilide, people with diabetes may have increased blood sugars.
Dental concerns of thiazide diuretics: Dizziness when standing after sitting or lying (postural hypotension).7
Potassium-sparing diuretics: Potassium-sparing diuretics interfere with the sodium-potassium exchange in the distal convoluted tubule of a kidney cell. Potassium is an electrolyte that is important for function and transmitting nerve impulses, and making muscles contract. Some block the aldosterone receptor. They are relatively weak diuretics but may cause high potassium levels especially if used with other medications that retain potassium, such as ACE inhibitors. They can be used on their own but are most commonly used in combination with other diuretics.4
Other uses: Preventing hypokalemia, reduce ascites, and heart failure.7
- Dyrenium (Triamterene): Initial dose100 mg twice a day after meals. Maximum dose 300 mg a day.
- Midamor (Amiloride): Initial dose 5 mg once a day. Maintenance 5 to 10 mg once a day. Better tolerated than triamterene.
- Eplerenone (Inspra): Initial dose 25 mg once a day and increased dose to 50 mg if needed. Most are selective and less potent, leading to reduced side-effects, although more expensive.
- Spironolactone (Aldactone, CaroSpir): Initial dose 50 to 100 mg once a day or divided into two to four doses. May be increased to 200 mg a day. Most widespread use and less expensive.
Side effects with the combination of Amiloride and Triamterene: Stomachaches, headaches; diarrhea or constipation; skin rash; aches, pains, muscle cramps, and weakness; hyperkaliemia (high potassium levels); and sleepy or confused.
Side effects with the combination of spironolactone and eplerenone: Stomach upset and nausea; sexual problems; enlargement of breasts in both sexes; confusion; irregular menstrual cycles; excessive hair growth; hyperkaliemia (high potassium levels); skin rash; and liver problems.
Drug interactions and precautions for spironolactone and eplerenone: ACE inhibitors, angiotensin receptor antagonist.
Dental concerns of spironolactone and eplerenone: Xerostomia, postural hypotension.8
Loop diuretics: Loop diuretics are a potent diuretic due to the efficacy of the unique site of action involving the loop of Henle, a portion of the renal tubule. It increases the elimination of sodium and chloride by preventing reabsorption of sodium and chloride. Water is drawn into the nephron of the kidney, and urine volume increases.
Other uses: Edema and pulmonary edema, ascites, liver, and kidney failure.
- Bumetanide (Bumex): Usual dose .5 to 2 mg.
- Ethacrynic acid (Edecrin, Sodium Edecrin): 50 mg.
- Furosemide (Lasix): 40 mg twice a day, and if no results, another antihypertensive medication is added.
- Torsemide (Demadex): Initial dose 5 mg once a day. In four to six weeks, increase to 10 mg once a day if needed. Maximum dose 20 mg, and if needed, another antihypertensive medication is added.4,6
Side effects of loop diuretics: Sulfa sensitivities since these drugs are considered sulfa drugs; high uric acid, calcium, or hypercalcemia; low magnesium levels, dehydration; ototoxicity or hearing damage (reversible when the medication is stopped); and muscle cramps.
Drug interactions and precautions for loop diuretics: Cancer drugs, Platinol, aspirin, sulfa drugs, digoxin, diabetes medications, Tikosyn, and lithium.
Dental concerns of loop diuretics: Syncope, xerostomia, postural hypotension, and patients may need to use the restroom throughout the appointment.
Angiotensin II receptor blockers: Angiotensin II is a chemical in the body that causes muscles around the blood vessels to contract and narrow and cause high blood pressure. Angiotensin II receptor blockers (ARBs) relax the blood vessels, decreasing the narrowing of the blood vessels and improves blood flow to lower the pressure. Prescribed when ACE inhibitors are not tolerated.
Some ARBs need to be converted to an active form in the body before they lower blood pressure, suggesting some ARBs such as irbesartan and candesartan work better for lowering blood pressure.9 ARBs end in –sartan.
Other uses: To treat heart failure and prevent failure in people with diabetes and high blood pressure.
- Losartan (Cozaar): Initial dose 50 mg once a day. Maintenance 25 to 100 mg in one to two divided doses.
- Telmisartan (Micardis): Initial dose 40 mg once a day and then increased, if needed, up to 80 mg a day.
- Valsartan (Diovan, Prexxartan): Initial dose 80 to 160 mg once a day. Maintenance dose 80 to 320 mg once day.
- Olmesartan (Benicar): Initial dose 20 mg once a day and then increased, if needed, up to 40 mg a day.
- Candesartan (Atacand): Initial dose 16 mg once a day and then increased, if needed, up to 32 mg a day.
- Eprosartan (Teveten): Initial dose 600 mg once a day. Maintenance dose 400 to 800 mg in one to two divided doses.
- Irbesartan (Avapro): Initial dose 150 mg once a day and then increased, if needed, up to 300 mg a day.
- Azilsartan (Edarbi): Initial dose 40 mg once a day and then increased, if needed, up to 80 mg once a day.9
Side effects of angiotensin II receptor blockers: Hyperkalemia; low blood pressure; dizziness; headaches; indigestion; bronchitis, upper respiratory tract infections; flu-like symptoms; drowsiness, fatigue; increased blood glucose levels; sexual dysfunction; excessive coughing; and destruction of skeletal muscle.
Drug interactions and precautions for angiotensin II receptor blockers: Diuretics, other blood pressure medications, lithium, celecoxib, aspirin, and NSAIDs.10
Dental concerns of angiotensin II receptor blockers: Abnormal taste sensation (metallic or salty), postural hypotension, and sinus infections.
Angiotensin-converting enzyme inhibitors: Angiotensin-converting enzyme inhibitors (ACE inhibitors) widen the blood vessels to aid in easy blood flow and reduce blood pressure. They work by preventing the formation of angiotensin II. ACE inhibitors end in –tec, -pril, and -ace.
Other uses: Treating left ventricular dysfunction, heart failure, scleroderma, preventing strokes and kidney disease with high blood pressure or diabetes.
- Captopril (Capoten): Initial dose 25 mg two to three times a day one hour before meals. Maintenance dose increases after one to two weeks to 50 mg three times a day before meals. Maximum dose 450 mg a day. If still not responding, a thiazide diuretic may be added.
- Fosinopril (Monopril): Initial dose 10 mg once a day alone or in combination with a diuretic. Maintenance dose 20 to 40 mg once a day. Maximum dose 80 mg.
- Lisinopril (Prinivil, Zestril): Initial dose 5 to 10 mg once a day, Maintenance dose 20 to 40 mg once a day. Maximum dose 80 mg once a day.
- Ramipril (Altace): Initial dose 2.5 mg once a day with patients not taking a diuretic. Maintenance 2.5 to 20 mg once a day or divided doses.
Side effects of angiotensin-converting enzyme inhibitors: Dry, persistent cough; headaches, dizziness; chest pain; drowsiness, weakness; rash; and increased uric acid, creatine, blood urea nitrogen, and blood potassium levels.
Drug interactions and precautions for angiotensin-converting enzyme inhibitors: Aspirin, NSAIDs, lithium, and potassium supplements.
Dental concerns of angiotensin-converting enzyme inhibitors: Abnormal taste metallic and salty, loss of taste, and xerostomia.11
Beta-blockers: Beta-blockers, also known as beta-adrenergic blocking agents, help in reducing the heart rate when decreasing the blood pressure. They work by blocking the effects of the hormone epinephrine. Beta-blockers slow the heartbeat, which provides less force to the heart and opens up the veins and arteries to improve blood flow. Beta-blockers are usually prescribed for high blood pressure when other medications haven’t effectively worked.
Other uses: Angina pectoris, myocardial infarctions, heart attacks, and migraines.
There are three main types − non-selective, cardio-selective, and third-generation beta-blockers.
Non-selective beta-blockers act on all beta-blockers (beta-1 receptors with heart and kidney; beta-2 receptors with lung, blood vessel, stomach, uterus, muscle, and liver cells; and beta-3 receptors with fat cells).12
- Nadolo (Corgard): Initial dose 40 mg once a day and may need to be increased by 40 to 80 mg a day until achieved levels are felt. Maximum dose of 320 mg a day.12
- Propranolol (Inderal, InnoPran XL): Initial dose 40 mg twice a day. Maintenance dose 120-140 mg two to three divided doses a day. Maximum dose 640 mg a day.12,13
Selective beta-blockers are designed to target only beta-1 receptors in the heart cells and do not affect beta-2 receptors.
- Acebutolol (Sectral): Initial dose 400 mg once a day or 200 mg twice a day and, if needed, increase the dosage to 600 mg twice a day as needed. Maintenance ranges from 400 to 800 mg a day.
- Atenolol (Tenormin): Initial dose 50 mg once a day. Maintenance dose 50 to 100 mg once a day. Maximum dose 100 mg a day.
- Bisoprolol (Zebeta): Initial dose 5 mg a day. If needed, increase to 10mg a day. Maximum 20 mg a day.
- Metoprolol (Lopressor, Toprol XL): Metoprolol tartrate immediate, release tablet initial dose 100 mg once a day or divided doses. Maintenance dose 100 to 450 mg a day. Metoprolol succinate extended, release initial dose 25 to 100 mg once a day. Maximum dose 400 mg a day.
Third-generation beta-blockers have additional effects to further relax blood vessels and ease high blood pressure.12
- Carvedilol (Coreg): Initial immediate release dose 6.25 mg twice a day and maintain for seven to 14 days. Maintenance dose 12.5 mg twice a day for 10 to 14 days and, if needed, increase to 25 mg twice a day. Maximum dose of 50 mg. Initial dose for extended-release dose 20 mg once a day. Maintain for seven to 14 days. Maintenance dose 40 mg once a day for seven to 14 days and, if needed, increase dose. Maximum dose 80 mg.
- Labetalol (Normodyne): Initial dose 100 mg twice a day alone or added to a diuretic regimen. Maintenance dose 200 to 400 mg twice a day. Maximum dose of 2400 mg.
- Nebivolol (Bystolic): Initial dose 5 mg once a day. Increase dose at two-week intervals. Maximum dose of 40 mg once a day.13
Side effects of beta-blockers: Cold hands and feet; fatigue; weight gain; depression; shortness of breath; trouble sleeping, may trigger asthma attacks if asthma is present; block signs of low blood sugars; and increase cholesterol.
Drug interactions or precautions for beta-blockers: Calcium channel blockers, epinephrine and norepinephrine-depleting drugs, anesthetics, statins, NSAIDs, insulin and diabetic medications, muscle relaxers, and blood thinners.
Dental concerns of beta-blockers: Xerostomia, slows metabolism of lidocaine, bupivacaine, mepivacaine, inhibits the vasodilatory effect of epinephrine, and postural hypotension.12

They are usually not the first line of treatment for blood pressure and are used in combination with other drugs when blood pressure is challenging to control. Some alpha-blockers have a “first-dose effect,” meaning when it’s initially taken, it may cause low blood pressure, dizziness, and syncope when rising from a seated or lying position. This is why it’s prescribed to take at bedtime.
Other uses: To treat or improve an enlarged prostate in men.14
- Doxazosin (Cardura): Initial dose 1 mg once a day. Maintenance dose 1 to 16 mg once a day.
- Prazosin (Minipress): Initial dose 1 mg two to three times a day. Maintenance dose 1 to 20 mg per day in divided doses.
- Terazosin (Hytrin): Initial dose 1 mg once a day at bedtime. Maintenance dose increased slowly as needed 1 to 5 mg once a day.
Side effects of alpha-blockers: Dizziness, headaches, pounding heartbeat, and weakness.
Drug interactions and precautions of alpha-blockers: Beta-blockers, calcium channel blockers, medications for erectile dysfunction, histamines, and anxiolytics.
Dental concerns of alpha-blockers: Postural hypotension and decreased salivary flow.
Calcium channel blockers: Calcium channel blockers reduce the amount of calcium entering the heart muscles to reduce the heart rate in controlling the blood pressure. Calcium causes the heart and arteries to contract more strongly, so by blocking calcium, it allows blood vessels to relax and open for better blood flow.
Several types of calcium channel blockers have other uses, including coronary heart disease, angina arrhythmia, and circulatory conditions. Calcium channel blockers end in –dipine.
Other uses: Angina, abnormal heart rhythms, disease of the heart muscles, and migraines.
- Amlodipine (Norvasc): Initial dose 5 mg a day may be increased by 2.5 mg a day every seven to14 days, not to exceed 10 mg a day. Maintenance dose 5 to 10 mg a day.
- Felodipine (Plendil): Initial dose 2.5 to 5 mg once a day. Maintenance 2.5 to 10 mg once a day. Maximum dose 20 mg a day.
- Isradipine (DynaCirc): Initial dose 2.5 mg twice a day alone or with a diuretic. Maintenance dose increases to 5 mg a day at a two-to-four-week interval. Maximum dose of 20 mg a day.
- Nifedipine (Procardia XL, Adalat CC): Extended-release 30-60 mg once a day, may be increased every seven to 14 days as needed. Maximum dose 120 mg a day.15
Side effects of calcium channel blockers: Headaches; dizziness and drowsiness; rash, flushing; fluid retention; constipation, nausea; low blood pressure; and sexual and liver dysfunction.
Drug interactions and precautions for calcium channel blockers: Verapamil, diltiazem, other calcium channel blockers, and grapefruit.
Dental concerns of calcium channel blockers: Overgrowth of gum tissue (gingival hyperplasia), and gingiva can become lumpy, thick, and uneven, as well as xerostomia.16
Renin inhibitors: Renin inhibitors inhibits the enzyme that makes the production of angiotensin to constrict blood vessels. Renin converts angiotensinogen to angiotensin I, which is then converted to angiotensin II, which is the dangerous vasoconstrictor that causes blood pressure to rise.
Other uses: Used mainly just for high blood pressure.
- Aliskiren (Tekturna): Initial 150 mg once a day. Maintenance the dosage may be increased to 300 mg if blood pressure is not controlled.17
Side effects of renin inhibitors: Light-headedness; little or no urination; diarrhea; high potassium accumulation; and low levels of sodium.
Drug interactions and precautions for renin inhibitors: If diabetes is present, avoid other blood pressure medications, cyclosporine, NSAIDs, and itraconazole.
Dental concerns of renin inhibitors: Postural hypotension.
Central agonists: Central agonists lower the heart rate to reduce blood pressure. They block signals from the brain to the nervous system that speed up the heart and narrow the veins and arteries. It prevents the heart from pumping as hard and promotes blood flow easily. They are used in combination with other medications if blood pressure hasn’t been effectively lowered with central agonists alone.
A sudden stop in these medications can cause a dangerous increase in blood pressure.18
Other uses: ADHD, drug withdrawal, especially in opioid pain medications, hot flashes in menopause, and Tourette syndrome.
- Clonidine (Catapres, Kapvay): Initial dose 0.1 mg 2 times a day, morning and night. Maintenance dose 0.2 to 0.6 in divided doses. Maximum dose 2.4 mg in divided doses.
- Guanfacine (Intuniv): Initial dose 1 mg a day. Maintenance dose 1 to 7 mg. The doses are determined by the person’s weight.
- Methyldopa (Aldomet): Initial dose 250 mg two to three times a day. Maintenance 500 mg to 2 grams in divided doses two to four times a day. Maximum dose 3 grams a day. Hypertensive emergency: IV 250-500 mg over 30 to 60 minutes every six hours to a maximum of 1 gram every six hours.
Side effects of central agonists (These medications have strong side effects): Abnormally slow heart rate; constipation; drowsiness, sedation, fatigue; dizziness, headaches; fever; and impotence.
Drug interactions and precautions for central agonists: Abilify, Benadryl, Cymbalta, Lyrica, metoprolol, and Xanax.
Dental concerns of central agonists: Xerostomia and increased central nervous system depressant.
Vasodilators: Vasodilators opens blood vessels by affecting the muscle walls of the arteries and veins, preventing the muscles from tightening and the walls narrowing. Blood flows easily, reducing the heart’s workload and reducing blood pressure.
They act directly on the blood vessels as opposed to the hormones or nerves that control the blood vessels. There are three different modes of vasodilators. They work mainly in the arteries, veins, or both.
Some of these medications are used for heart failure and as hypertensive emergencies.19.20
Arterial vasodilators:
- Hydralazine (Apresoline): Initial dose 10 mg 4 times a day for the first two to four days, then increase to 25 mg four times a day for the first week. Second week and after increase dosage to 50 mg four times a day. Maintenance dose is at the lowest effective levels.
- Minoxidil (Loniten): Initial dose 5 mg once a day. Maintenance dose 10, 20, 40 mg once or a day or divided doses. Effective dose range is 10 to 40 mg. Maximum dose is 100 mg a day.
Venous vasodilators (organic nitrates):
- Nitroglycerin (Nitrostat, Nitro-Bid, Nitro-Quick): Occurs in sublingual, transdermal, spray, ointment, and capsule transmissions. Doses vary depending on the route of transmission.
- Amyl nitrate: Used by inhalation to relive the pain of an angina attack and comes in a pre-dosed 0.3 ml glass capsule. Move it back and forth under the nose and inhale the vapor one to six times. Doses may be repeated within one to five minutes. If pain is not relieved after two doses in a 10-minute period, go to the hospital.
- Isosorbide dinitrate (Isordil): Sublingual dose 2.5 to 5 mg used 15 minutes prior to a likely cause for an anginal episode. Initial dose immediate release 5 to 20 mg two to three times a day. Maintenance dose 10 to 40 mg two to three times a day.
Mixed vasodilators:
- Sodium nitroprusside (Nitropress): Used in hypertensive emergencies by infusion.
- Terazosin (Hytrin): Initial dose 1 mg at bedtime. Maintenance dose if needed increased from 1 mg to 5mg maximum dose 20 mg.
- Prazosin (Minipress): Initial dose 1 mg two or three times a day. Maintenance dose 1 to 20 mg in divided doses. Maximum dose 40 mg per day in divided doses while therapeutic doses range from 6 to 15 mg.
Side effects of vasodilators: Chest, muscle, and joint pain; excessive hair growth, hair becomes darker or thicker; flushing, rashes; vomiting, nausea; fluid retention; and heart palpitations, rapid heartbeat.
Drug interactions and precautions for vasodilators: Nitrates, thiazides, corticosteroids, oral contraceptives, and chlorpromazine.
Dental concerns of vasodilators: Postural hypotension, epinephrine (may cause tachycardia).19,20
There are a lot of medications to treat high blood pressure, and they can be confusing. Blood pressure medication is not a cure − only a treatment to control it. Patients most likely will be on medication for life, and if it is not treated, it can cause serious conditions such as heart failure, blood vessel disease, stroke, or kidney disease.

Need CE? Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- What is High blood Pressure? (2016, October 31). American Heart Association. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/what-is-high-blood-pressure.
- High Blood Pressure (hypertension). (2021, January 16). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410.
- Types of Blood Pressure Medications. (2017, October 31) American Heart Association. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications.
- Fookes, C. (2018, May 15) Diuretics. com. Retrieved from https://www.drugs.com/drug-class/diuretics.html.
- Multum, C. (2020, September 28) Diamox. com. Retrieved from https://www.drugs.com/mtm/diamox.html.
- Ogbru, A. (n.d.). Diuretics. Retrieved from https://www.rxlist.com/diuretics/drug-class.htm.
- Knott, L. (2020, May 26). Thiazide Diuretics. Retrieved from https://patient.info/heart-health/high-blood-pressure-hypertension/thiazide-diuretics.
- Knott, L. (2020 May 26). Potassium-sparing Diuretics. Retrieved from https://patient.info/digestive-health/dietary-potassium/potassium-sparing-diuretics.
- Ogbru, O. (2019, December 20). Angiotensin II Receptor Blockers (ARB). Medicine Net. Retrieved from https://www.medicinenet.com/heart_health_pictures_slideshow/article.htm.
- Sinha, S. (2020, November 25) Losartan. com. Retrieved from https://www.drugs.com/losartan.html.
- Ogbru, O. (2019, October 17). ACE Inhibitors Drug Class Side Effects List of Names, Uses, and Dosage. Medicine Net.Retrieved from https://www.medicinenet.com/ace_inhibitors/article.htm.
- Vandergriendt, C. (2020, February 12). What are the Side effects of Beta-Blockers? Retrieved from https://www.healthline.com/health/beta-blockers-side-effects.
- Beta Blockers. (2019, August 16). com. Retrieved from https://www.drugs.com/mca/beta-blockers.
- Alpha Blockers. (n.d.). com. Retrieved from https://www.drugs.com/mca/alpha-blockers.
- Ogbru, A. (n.d.). Calcium Channel Blockers (CCBS). Rx list. Retrieved from https://www.rxlist.com/calcium_channel_blockers_ccbs/drug-class.htm.
- Can Blood Pressure Medications Impact Your Oral Health? (n.d.). Momentum Insurance Plans. Retrieved from https://www.momentumplans.com/MadisonDentalInsuranceNews/can-blood-pressure-medication-impact-oral-health.
- Multum, C. (2020, January 20). Aliskiren. Drugs, com. Retrieved from https://www.drugs.com/mtm/aliskiren.html.
- Central-acting Agents. (2019, August 14). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure-medication/art-20044451.
- (2019, January 09). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure-medication/art-20048154.
- Amyl Nitrate (Inhalation Route). (2020, November 01). Mayo Clinic. Retrieved from https://www.mayoclinic.org/drugs-supplements/amyl-nitrite-inhalation-route/proper-use/drg-20061803.











