The scientific journal Nature Communications recently published a breakthrough study that is poised to further advance the field of regenerative dentistry. The study unveiled new information about the dental cell type atlas and other mechanisms necessary to reconstruct and engineer teeth. Based on their findings, it is highly likely the information provided by the research will likely encourage further studies of the cell dynamics involved in reparative and regenerative therapies.
About Regenerative Dentistry
Regenerative dentistry uses a combination of chemical, biological, and physical engineering to restore and improve a patient’s dental health. Professionals can use regenerative dentistry procedures to renew or replace damaged gingival tissue, bones, and teeth by regrowing them with autologous stem cells.
Regenerative Dentistry Procedures and Ideal Candidates
Common procedures include bone and gingival tissue regeneration. Pocket reduction, non-surgical periodontal therapy/SRP also fall under the same umbrella of regenerative dentistry. Natural bone regeneration is ideal for candidates who have deteriorated jawbones and need dental implants. Gingival tissue regeneration helps patients who need an additional layer of membrane to support their existing teeth or implants. A successful pocket reduction procedure may prevent the loss of gingival tissue by killing and removing harmful bacteria subgingivally using instrumentation and antimicrobial solutions.
Regenerative dentistry may be a suitable treatment plan for a variety of patients who have experienced bone loss and damaged gingiva due to advanced stages of periodontal disease. People who have recently lost a tooth or maybe at risk of tooth loss may also be potential candidates.
For the study, the researchers used genetic tracing and an unbiased single-cell RNA sequencing method to examine every cellular subtype’s heterogeneity and plasticity associated with the teeth. They also dissected the complex nature of terminal and transient cell states, which allow teeth to self-regenerate.
About the Global Clinical Study
A team of scientists from Austria, Sweden, and the United States collaborated to further understand the cell types and mechanisms of dental growth necessary to engineer teeth. Together, the researchers examined the cellular composition of growing and non-growing teeth from lab mice and humans at the Medical University of Vienna, Karolinska Institutet, and Harvard University. The human teeth were extracted from patients at a variety of clinics and hospitals, including the Department of Oral Surgery at the Medical University of Vienna.
For the study, the scientists used genetic tracing and an unbiased single-cell RNA sequencing method to examine the heterogeneity and plasticity of every cellular subtype associated with the mouse and human teeth. They also dissected the complex nature of terminal and transient cell states, which allow teeth to self-regenerate.
In Conclusion
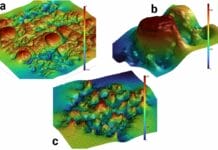
By the end of the study, the scientists were able to develop detailed atlases of mouse and human teeth that may expand the field of regenerative dentistry. A few of their discoveries included the subtypes of stellate reticulum and certain ameloblasts, which can help express several mechanotransduction-related genes in mice and humans.
The researchers revealed they were able to identify the different pathways stem cells and adult cells take as they form into odontoblasts, dentin, and tooth enamel. Besides deciphering this complicated process and discovering new cell types, the scientists were also able to better understand how the cell layers within a patient’s teeth can impact its overall sensitivity. The team of researchers strongly believe their findings will be useful for future scholars interested in regenerative biology. The results of their efforts are online and publicly available to the scientific community.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.