
Eagle syndrome is a rare condition where the styloid process becomes elongated or the stylohyoid ligaments become calcified. When the process elongates, it can constrict nerves, the carotid artery, and create a variety of symptoms that are often misdiagnosed. (see Image 1 and 2)
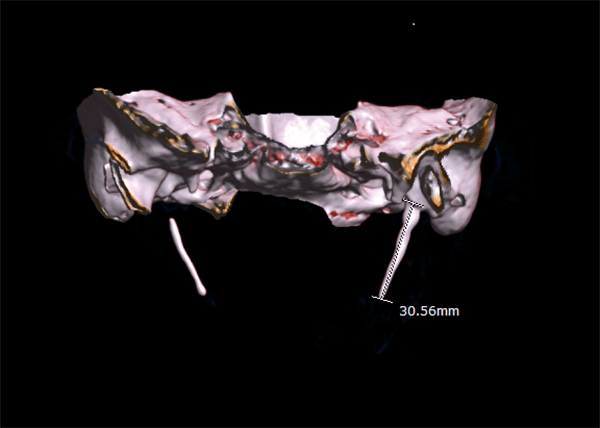
Image courtesy Dr. Jadon Ashok, CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0, via Wikimedia Commons.
The condition was discovered by Dr. Watt W. Eagle in 1937, an otolaryngologist at Duke University. The styloid process is a pointed process of the temporal bone that anchors several muscles affiliated with the tongue and larynx.1,2 The normal styloid process is approximately 2.5 cm on average.
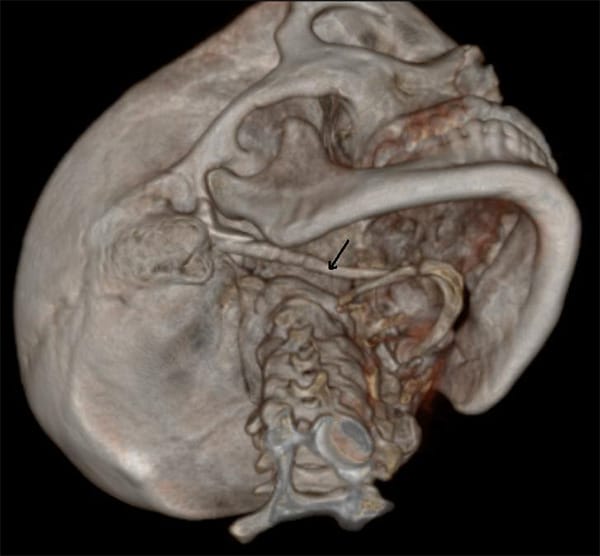
Image courtesy Benutzer:MBq, via Wikimedia Commons.
The common symptoms of Eagle syndrome are:1,2
- Recurrent pain in the middle part of the throat
- Tinnitus (chronic ringing in the ear)
- Neck and/or facial pain
- Chronic, dull throat pain that radiates to the ear and exacerbates with the turning of the head
- A feeling of thickness in the throat or difficulty swallowing
- Headache
- Dizziness
Causes of Eagle Syndrome
Although Eagle syndrome is considered a rare disease, syndrome, or disorder, it has been discovered in patients following throat trauma or tonsillectomy.1 Perhaps the trauma of injury or tonsillectomy surgery causes the body to create a thickening of the ligaments as a way to protect the area, much like scar tissue. Could the body’s inflammatory response to such injury cause the styloid process to lengthen?
Unrelated to trauma or tonsillectomy, another form of Eagle syndrome contributes to dizziness and headaches as the elongated styloid process or calcified stylohyoid ligament compresses the carotid artery.1,2 In rare and severe instances, the carotid artery’s compression can lead to stroke or even death.5
The actual cause for, and progression of, Eagle syndrome is not known. Abnormal bone metabolism and developmental anomalies are thought to be involved.3
An evaluation for Eagle syndrome calls for asking the right questions, such as:
- “Have you ever been injured in the throat?”
- “Have you had a tonsillectomy?”
- “Does it hurt when you rotate your head?”
- “Do you have difficulty swallowing?”
- “Do you have ringing in your ears?”
- “Do you have throat pain that radiates to your ear(s)?”
- “Do you have pain in your neck/throat region?”
- “Do you have frequent headaches?”
- “Have you been experiencing dizziness?”
Radiographic Imagery
Is the styloid process approximately 2.5cm, or has it elongated? How does the TMJ look? If the styloid process is elongated and the TMJ looks relatively normal, a referral to an ear, nose, and throat specialist (ENT) is advised.

The ideal radiologic review is with 3D computed tomography. However, many dental offices do not have this imagery available.4 The referral to an ENT for further examination should be recommended if a patient does not respond to TMD therapy, NSAIDs, or when radiographs do not reveal any significant temporal mandibular disorder (TMD) issues.
Most symptoms associated with Eagle syndrome are also commonly found symptoms of TMD, making diagnosing Eagle syndrome a little tricky. As a general rule, the dental profession has been taught to evaluate for TMD and treat accordingly. A second review of panoramic images in patients who find little comfort with TMD treatment should be considered. A closer look may reveal an elongation of the styloid process, prompting a referral to an ENT.
However, if your patient has no problematic symptoms and you notice an elongation of the styloid process on panoramic imagery, inform the patient of your finding and advise of the potential for Eagle syndrome symptoms as this discovery in itself does not diagnose the syndrome.
Conditions commonly misdiagnosed instead of Eagle syndrome are:
- TMJ dysfunction
- Otitis media
- Atypical migraine
- Pathologies of third molars
- Trigeminal neuralgia
- Fibromyalgia
Treating Eagle Syndrome
Eagle syndrome is not treated in the dental setting. The best recommendation is a referral to an ENT for evaluation where they can properly diagnose, treat, or refer to a recommended specialist. Eagle syndrome can be initially treated with NSAIDs, steroids, or physical therapy.5 For some that is enough to reduce inflammation and pain, bringing comfort. If dizziness or headaches persist or pain levels do not diminish, surgical intervention should be considered as the carotid artery is most likely being compressed.
Surgical intervention (styloidectomy) can be done either intraorally via the tonsillar fossa or extraorally via the neck. As you can imagine, intraorally will not leave a visible scar but can be dangerous as the vascular nature causes poor visibility of the surgical site. Extraoral surgery from the neck aspect will leave a noticeable scar but allows for better visibility during the procedure. There is an additional risk of facial nerve damage via the extraoral approach. Due to the compromising nature of each procedure, the skill level and comfort of the surgeon will determine which approach is to be used.5
The next time you have a patient complaining of head and neck aches and pains, ask the right questions and obtain a panoramic image. Does their styloid look normal, or is it elongated? TMD pain usually lasts a long time, whereas pain from Eagle syndrome may last only a few seconds upon turning the head.
A 2014 article in Clinical Medicine and Diagnostics offered the helpful guide below to show a differential diagnosis of Eagle syndrome. The authors’ intent was to take some of the guesswork out of diagnostic referrals.5
TMD
Pain: A dull, stabbing pain of moderate intensity that lasts minutes to hours; the TMJ/muscle pain includes an inability to open the mouth and pain during mastication.
General treatment: NSAIDs.
Local treatment: Physical therapy, splints, anesthetic injections.
Idiopathic Trigeminal Neuralgia
Pain: Pain with severe intensity that lasts seconds, usually a trigger zone.
General treatment: Anti-convulsants.
Local treatment: None
Eagle Syndrome
Pain: A dull, medium intensity pain of short duration, especially upon turning head; pain in neck, throat, the floor of the mouth, ear, headache, dizziness.
General treatment: NSAIDs.
Local treatment: Corticoid injection, surgery (internal or external approach).
Conclusion
In summary, Eagle syndrome can mask itself as temporal mandibular disorder, among other things – easily being misdiagnosed and mistreated. Use the guide above to assist with differential diagnosis and expose clear, diagnostic panoramic images. The next time a dental patient complains of TMD-like pain, ask the appropriate questions, review their panorex, and refer as needed.
Need CE? Click Here to Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Eagle syndrome. (2017, April 18). S. Department of Health & Human Services: National Institutes of Health. Retrieved from https://rarediseases.info.nih.gov/diseases/9401/eagle-syndrome
- Rinaldi, V. (2016, May 6). Eagle Syndrome. Medscape. Retrieved from http://emedicine.medscape.com/article/1447247-overview#a6
- Zuber, M., Meder, J., Mas, J. Carotid Artery Dissection Due To Elongated Styloid Process. Neurology. 1999; 53(8): 1886. DOI: 1-.1212/WNL.53.8.1886. Retrieved from https://doi.org/10.1212/WNL.53.8.1886
- Valerio, C., Peyneau, P., de Sousa, A., et al. Stylohyoid Syndrome: Surgical Approach. J Craniofac Surg. 2012; 23(2): e138-e140. DOI: 10.1097/SCS.0b013e31824cdb46.PMID:22446450. Retrieved from https://pubmed.ncbi.nlm.nih.gov/?term=Cardoso=FO&cauthor_id=22446450
- Chickooree, D., Ram, V. (2014) Eagle’s Syndrome – View from the General Practitioner’s Perspective. Clinical Medicine and Diagnostics. 2014; 4: 9-13. DOI: 10.5. Retrieved from https://www.semanticscholar.org/paper/Eagle%E2%80%99s-Syndrome-View-from-the-General-Perspective-Chickooree-Ram/b8e71f92b5367713d91393bdad41de65710bd012
- Kaushik, A., Tanwar, R., Garg, P., et al. Calcified Sylohyoid Ligaments: A Diagnostic Dilemma. SRM Journal of Research in Dental Sciences. 2012; 3(4): 275-278. Retrieved from https://www.srmjrds.in/article.asp?issn=0976-433X;year=2012;volume=3;issue=4;spage=275;epage=278;aulast=Kaushik#










