Eagle syndrome (stylohyoid syndrome) is within the category of many other conditions since there are no definite known causes. Pain is experienced in the head and neck region, and the symptoms can mimic other conditions that cause head and neck pains.
Tonsillectomies are considered a likely factor as a result of possible scarring and injury from the procedure. Other factors may be abnormal angular position and size of the styloid process, ossification of muscular tendons and stylohyoid ligament, or an injury to the area that never fully healed. Other known contributors are an elongated styloid process or calcified hardening of the stylohyoid ligament.
The styloid process is the small pointy bone located right below the ear. A normal styloid process is 2.5 to 3 cm in length. Any longer than 3 cm is considered elongated, which can spontaneously arise over time. The result of the elongation often causes pain in the ear, neck, head, mouth, throat, and face.
Eagle syndrome affects women more than men and is more common between 40 to 60 years of age. While 4% of the population has an elongated styloid process, and within this range, 4% of these cases have symptoms.1
Eagle syndrome is characterized by two types.
Classic ‒ Classic eagle syndrome is mainly unilateral, but it could be bilateral in rare cases. They are usually seen after throat trauma, injury to the neck or pharynx, or after a tonsillectomy or other neck surgeries. Secondary issues of a tonsillectomy within classic syndrome are stimulation of the cranial nerves 5, 7, 9, and 10 and their associated branches. Scarring near the styloid apex can cause compression or stretching of the nerve structures near the styloid process. This results in a sore throat, tinnitus, neck, ear, and/or facial pain.
Vascular ‒ Vascular (or carotid artery) eagle syndrome is originated when the elongated styloid process impinges the internal carotid artery. In these cases, when compression is applied, such as turning the head, it can tear inside the blood vessel to restrict blood flow and increase an transient ischemic attack (TIA) or a stroke. Other main symptoms for vascular Eagle syndrome may be the same as classic eagle syndrome with the addition of syncope, dizziness, nausea, vision issues, and stroke symptoms.1
Complications
In some cases, a long styloid process is able to put pressure on the internal carotid arteries. Carotid arteries are bilateral on the anterior of the neck, and there are external and internal carotid arteries. External carotid arteries bring blood to structures outside of the skull. Internal carotid arteries bring blood inside the skull, such as the brain. When there’s pressure on the internal artery, it can cause a stroke.
Differential Diagnosis
Eagle syndrome is affected by different nerves and vascular structures, making it clinically confusing to other conditions, and it may mimic other syndromes that involve the cranial nerves (trigeminal neuralgia and glossopharyngeal neuralgia). Neuralgias tend to arise from branches of one cranial nerve, while eagle syndrome arises from the distribution of multiple nerves and vascular structures. The complexity of symptoms depends on the various structures which are involved.2
Other resembling conditions are third molar impaction, temporomandibular joint disorders, migraines or headaches, arthritis in the cervical vertebral, atypical facial pain, inflammation of the tonsils and temporal arteries.1
Nerves
The different nerves that are affected play important roles in the symptoms (see Table 1 below).2
| Cranial Nerves (CN) | Location | Effects |
| CN VII facial nerve | Styloid process lies anterior to the facial nerve | VII carries pain fibers from the external auditory canal to cause ear pain |
| CN IX glossopharyngeal nerve | Stylohyoid ligament lies adjacent to the glossopharyngeal nerve | Responsible for pain fibers of the posterior pharynx to cause pain throat and swallowing pain. |
| CN XI (spinal accessory nerve), X (Vagus nerve), IX (glossopharyngeal nerve) form the pharyngeal plexus | At the cranial portion of the spinal accessory nerve | Compression of this plexus causes dysphagia |
| CN X Vagus nerve | Lies lateral to the stylohyoid ligament | Branchiomeric motor branches are responsible for phonation, and compression may cause hoarseness. |
| CN XII hypoglossal nerve | Travels lateral to the stylohyoid ligament | Causes tongue weakness and inability to protrude the tongue fully |
| CN V trigeminal nerve branches | Crosses the face | Irritation of this nerve causes facial and TMJ pain, jaw muscle spasms, and weakness. Obstruction causes the inability to open the mouth. |
Table 1 Cranial nerves. Chart courtesy Lara James.
Symptoms
Symptoms can mimic other conditions associated with orofacial pain. The News-Medical.Net website identifies some of these symptoms as:
- Mainly unilateral but can be bilateral pain with the face or neck and near the jaw
- Persistent pain that lasts a while, worse when yawning or turning the head or protrusion of the tongue
- Nagging, dull pain, or sharp shooting pain in the ear, head, neck, and face
- Ringing or buzzing in the ears
- Difficulty in swallowing
- Feeling as if something is stuck in the throat
- Hoarseness or voice alteration
- Extreme drooling or salivation
- Teeth and jaw pain3
Diagnosis
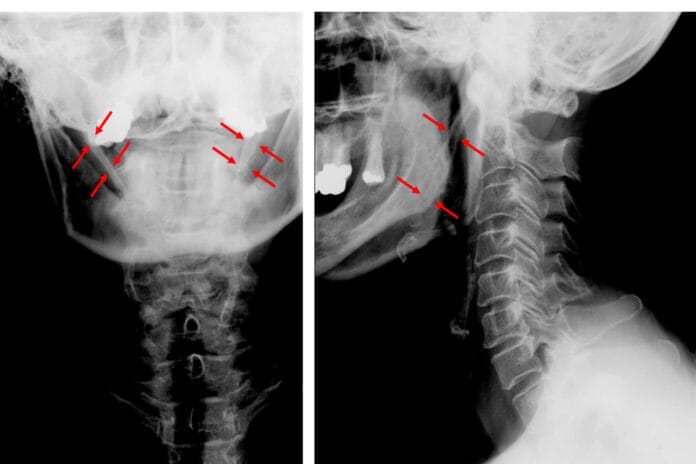
A thorough examination through physical evaluation and imaging is needed to eliminate other conditions and confirm eagle syndrome. To firmly confirm eagle syndrome is through imaging within the standard protocol through radiographs or CT. In dentistry, it can be seen on a panoramic radiograph (see Figure 1) and then referred to their physician for further evaluation.
An elongated styloid process can be palpated and felt intraorally versus a normal length one is not palpable. A gentle pressure with the index finger softly pushing over the tonsillar fossa. If this pressure results in pain at the location or is referred to the face, head, neck, or ear, it can be a sign of an elongated styloid process.1

Treatment
Nonsteroidal anti-inflammatory medication is used to relieve pain in mild cases. Other medications may include tricyclic antidepressants, anticonvulsants, steroids, and local anesthetics.4
In severe cases and the recurrence of pain, removal or shortening the styloid process through surgery is necessary. Surgery can be accomplished intraoral through the mouth or extraoral through the outside of the neck. If it’s an intraoral surgery, the tonsils are usually removed to access the styloid process. Although there are risks to major vessels, this technique is safe and simple and eliminates an external scar.
The external approach has better access to the styloid process and surrounding structures. Although there is better access as it requires going through the neck and connective tissue, a scar is definite, and there is an increased risk of trauma to neck structures (nerves, arteries, muscles). In recent years, the endoscope-assisted approach has become more routine. Most people recover with no remaining symptoms.4
Patients will have many aches and pains within the head region, and there are many conditions, and eagle syndrome is one more avenue to explore. Being aware of eagle syndrome and what to look for on a panoramic image can provide the patient with another possible explanation for pain. Although the condition is rare, it’s possible.
Need CE? Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Nedunchezhian, K. Eagle Syndrome – An Overview. SA Journal of Radiology. 2017; 21(1). Retrieved from http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S2078-67782017000100021
- Dunn-Ryznyk, L.R., Kelly, C.W. Eagle syndrome: a rare cause of dysphagia and head and neck pain: a male patient with a history of a motor vehicle accident presented with an unusual combination of symptoms, including sharp pain, jaw spasms, and chronic headache. Journal of the American Academy of Physicians Assistants. 2010; 23(12). Retrieved from https://go.gale.com/ps/i.do?p=AONE&u=googlescholar&id=GALE|A250215044&v=2.1&it=r&sid=AONE&asid=bbf8f979
- Mandal, A. (2019 June 28) What is Eagle Syndrome? Medical News Life Sciences. Retrieved from https://www.news-medical.net/health/What-is-Eagle-Syndrome.aspx
- Eagle Syndrome. (2021, January 19). NIH: Retrieved from https://rarediseases.info.nih.gov/diseases/9401/eagle-syndrome