Test Your Ultrasonic Scaling Knowledge!
Disclosure: We value transparency at Today’s RDH. This quiz is sponsored content from Dentsply Sirona Preventive as part of our sponsored partner program.
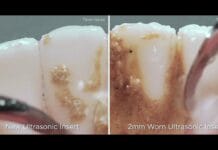
As an ultrasonic insert tip wears, a single millimeter of wear reduces efficacy by ____. A loss of 2 mm reduces efficacy by ____.
As an ultrasonic insert tip wears from use over time, this loss of tip length translates into a loss of efficacy. Research shows a single millimeter of wear reduces efficacy by 25%.1 A loss of 2mm reduces efficacy by 50%.1 Worn tips can cause the use of excessive pressure while scaling, which results in discomfort for both the clinician and patient.
A clinician should monitor the wear of ultrasonic insert tips often and use the wear guide supplied by the manufacturer to help monitor the need for replacement. The stack of an ultrasonic insert should be monitored as well. Spread, bent, or broken laminates in the stack can lead to loss of power and can damage the handpiece.
1. Lea, S.C., Landini, G., Walmsley, A.D. (2006). The Effect of Wear on Ultrasonic Scaler Tip Displacement Amplitude. J Clin Periodontol, 33, 37-41.
A triple bend ultrasonic insert is efficient at removing moderate to heavy calculus. The bends allow this insert to adapt well in periodontal pockets >4mm.
The beveled edge of a triple bend ultrasonic insert is efficient at removing moderate to heavy calculus. However, because of the bends, this insert does not adapt well in pockets >4mm and will cause significant damage to root and tooth structure if the point of the tip comes into direct contact at 90°. A triple bend ultrasonic insert is indicated for patients with moderate to heavy calculus, but not deep periodontal pockets.[1]
[1] Retrieved from https://www.dentsplysirona.com/content/dam/dentsply/microsites/cavitron_CA/GettingtheMostoutofUltrasonicScaling.pdf
Slim ultrasonic inserts should be used at a high power setting. Slim ultrasonic inserts are effective at removing both biofilm and heavy calculus.
Slim ultrasonic inserts should be used in accordance with manufacturer instructions, at a low to medium power setting. If used at high power settings, root structure can be compromised, and clinical attachment loss can occur. Trying to remove heavy calculus at a high power setting may also cause damage to the insert itself which can result in ineffective oscillation. Slim ultrasonic inserts, when used at the correct power setting, are effective at removing biofilm and light to moderate calculus. [1] [2]
[1] Casarin, R., Bittencourt, S., Del Peloso Ribeiro, E., Humberto, Nociti, F., Sallum, A., & Casati, M. (2010, March). Influence of Immediate Attachment Loss during Instrumentation Employing Thin Ultrasonic Tips on Clinical Response to Nonsurgical Periodontal Therapy. Quintessence International, 41(3), 249-256. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/20213026.
[2] Khambay BS, Walmsley AD, (1999, June). Acoustic Microstreaming: Detection and Measurement around Ultrasonic Scalers. J Clin Periodontology, 70(6), 626-631. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10397518.
A 30 kHz ultrasonic insert completes 60,000 strokes per second.
"Tip oscillation frequency is a measure of the number of times, per second, the ultrasonic scaler probe (tip) completes one whole oscillation cycle. During this cycle, the probe (tip) traverses the tooth twice, producing a forward and backward stroke. Therefore, a probe (tip) with a frequency of 30 kHz, performs 60,000 cleaning strokes per second, generally speaking." [1]
[1] Lea, S.C., Walmsley, A.D. (2011). Do Ultrasonic Scaler Inserts and Generators From the Same Manufacturer Optimize Performance? Annual Clinical Journal of Dental Health, 1, 22-27. Retrieved from https://cdn.vivarep.com/contrib/va/documents/al_lib_24.201272595235770.pdf
Benefits of the use of ultrasonic instrumentation include:
Benefits of the use of ultrasonic instrumentation include cavitation, lavage, precise mechanical movement, conservation of cementum, acoustic streaming, and acoustic turbulence.[1][2][3]
Cavitation: action created by the formation and collapse of bubbles in water by high-frequency sound waves surrounding an ultrasonic tip.[4]
Lavage: the therapeutic washing of the pocket and root surface to remove endotoxins and loose debris.[4]
Acoustic turbulence: agitation in the fluids surrounding a rapidly vibrating ultrasonic tip; has potential to disrupt the bacterial matrix.[4]
Acoustic microstreaming: Removal/disruption of biofilm by turbulent currents of water surrounding the tip.[5]
1. Jensen, S., Ayna, M., Hedderich, J., Eberhard, J. (2004). Significant Influence on Scaler Tip Design on Root Substance Loss Resulting from Ultrasonic Scaling: A Laserprofilometric in vitro Study. J Clin Periodontol, 31, 1003-1006. Retrieved from http://www.dr-ayna.de/downloads/journal_paradontologie.pdf.
2. Khambay, B.S., Walmsley A.D. (1999, June). Acoustic Microstreaming: Detection and Measurement around Ultrasonic Scalers. J Clin Periodontology, 70(6), 626-631. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10397518.
3. Walmsley, A.D., Lea, S.C., Felver, B., King, D.C., Price, G.J. (2013). Mapping Cavitation Activity around Dental Ultrasonic Tips. Clin Oral Invest, 17, 1227-1234. Retrieved from https://purehost.bath.ac.uk/ws/portalfiles/portal/5867057.
4. Wilkins, E. (2009). Clinical Practice of the Dental Hygienist (10th ed.). Baltimore, MD: Lippincott Williams & Wilkins.
5. George, M.D., Donley, T.G., Preshaw, P.M. (2014). Ultrasonic Periodontal Debridement: Theory and Technique. Ames, IA: John Wiley & Sons, Inc.