Test Your Polishing Knowledge!
Disclosure: We value transparency at Today’s RDH. This quiz is sponsored content from Dentsply Sirona Preventive as part of our sponsored partner program.
It is acceptable to polish every patient, and all teeth, with coarse paste.
“Dental hygienists who have adopted this method will use either whatever grit is available or coarse polishing paste on everything. Both are unethical because they ignore the patient's needs and could severely damage esthetic restorations. The premise for the "coarse polishing paste on everything" approach is that the use of the coarsest polishing paste available will remove the heaviest amounts of stain as well as the lightest amounts, therefore saving time. Providers who polish in this ill-advised fashion ignore the science of abrasion, which is to use the polishing grits in a progression of coarse, medium, and fine applications, changing the rubber cup with each grit size. Unfortunately, the "coarse paste on everything" approach is widespread as demonstrated by the fact that 80% of all prophylaxis pastes sold in the United States is coarse grit, followed by 10% in medium grit, and 10% in fine grit.1”
1. Barnes, C.M. (2012). Shining a New Light on Selective Polishing. Dimensions of Dental Hygiene. Retrieved from https://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1011&context=dentistryfacpub.
The redefined term, selective polishing, describes polishing all teeth, stained or unstained, but using the least abrasive polishing agent based on individual patient need.
In 1976, the term selective polishing was first introduced in the 4th edition of Clinical Practice of the Dental Hygienist by Esther Wilkins, DMD, RDH, BS. The technique of polishing only stained teeth was in response to a study which found 4 µm of enamel was removed during a 30-second polishing procedure with a pumice-water slurry. However, this study has since been disputed due to uncontrolled variables, small sample size, and the polishing technique did not accurately reflect clinical procedures.1
In 2012, Wilkins redefined the term in the 11th edition of Clinical Practice of the Dental Hygienist. Selective polishing now means to polish all teeth, stained or unstained, using the least abrasive polishing agent to meet a patient’s individual needs.1 Further, if coarse grit is used, to avoid abrasion which produces rough surfaces which accelerate staining and biofilm adherence, it should be followed by polishing with a medium grit, and finished with a fine grit, leaving the tooth as smooth as possible.2
1. Barnes, C.M. (2012). Shining a New Light on Selective Polishing. Dimensions of Dental Hygiene. Retrieved from https://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1011&context=dentistryfacpub.
2. Darby, M. (2012). An Evidence-Based Approach to Polishing Teeth. American Academy for Oral-Systemic Health. Retrieved from http://aaosh.org/evidence-based-approach-cleansing-polishing-teeth/.
To achieve a polished surface, particles must be 1-2 units more abrasive on the Mohs Hardness Scale* than the substrate being polished. The Mohs Hardness Value of enamel is 8.
*The Mohs Hardness Scale is a 10-point scale of mineral hardness; 1 being the softest, 10 being the hardest.
Multiple factors play into how abrasive a particular prophy paste is including the grit material’s hardness, particle size, and shape. The hardness of an abrasive material is measured by the Mohs Hardness Scale, with 1 being the softest and 10 being the hardest. “To achieve a polished surface, particles must be 1-2 units on the scale harder than the substrate being polished. To achieve a cleansed surface and to prevent scratching, the abrasive should be less than or equal in hardness to the surface being cleansed.1” Enamel has a Mohs Hardness of 5-6; other values include1:
Mohs Value | Material |
1 | talc |
2-4 | gold, cementum, dentin |
4-5 | amalgam |
5-6 | enamel, glass ionomer cements |
5-7 | composite resins |
6-7 | porcelain ceramics |
10 | diamond |
“The smaller (finer) the grit, the smaller the scratches, which means the shinier the tooth or restoration surface will be after polishing. The finest grit yields the least amount of abrasion, even if the abrasive material is high on the Mohs Hardness Scale. This explains why some agents have high Mohs Hardness Values, yet are used on substrates with low Mohs Hardness Values.1” Mohs Values of some abrasives used in dentistry include1:
Mohs Value | Abrasive |
0.4 | Potassium: cleansing agent in dentifrices and desensitizing agents, promotes occlusion of dentinal tubules. |
0.5 | Sodium: cleansing agent in denitrifies, used in some fluoride compounds |
2.0 | Aluminum silicates: cleansing and polishing agent, compatible with dental fluoride compounds |
2.0 | Glycine |
2.5 | Sodium bicarbonate |
3.0 | Calcium carbonate: mild abrasive used to polish teeth, gold foil, and plastic materials |
2.5-3.5 | Aluminum trihydroxide |
5.0 | Phosphate salts: such as pyrophosphate, dibasic calcium phosphate dehydrate, tricalcium phosphate, sodium metaphosphate; found in dentifrices |
5-6 | Rouge: used for polishing gold and precious metal alloys in lab, not to be used in the mouth |
6.0 | Calcium sodium phosphosilicate: the hardest of powders available for air polishing |
6-7 | Pumice: superfine pumice (pumice flour) and fine, medium, coarse pumice; used to polish teeth, gold foil, amalgam, and acrylic resin |
6-7 | Tin oxide: used to polish teeth and metallic restorations |
6-7 | Silica/Sand: such as hydrated silica, sodium potassium aluminum silicate |
6.5-7.5 | Zirconium silicate |
6.5-7.5 | Garnet: Used for polishing acrylic dental appliances and composites |
7.0 | Cuttle: used to coat paper disks to finish gold alloys, acrylics, and composites |
9.0 | Corundum: porcelain restorations and custom trays |
9.5 | Silicon carbide: used as an abrasive in coated discs, can cut metal alloys, ceramics, and plastic materials |
10 | Diamond: resin-based composite materials, metal backed abrasive strips, furcation files |
“With so many substrates in the oral cavity that require independent maintenance, there is not one prophylaxis paste that is suitable for all. Depending on the characteristics and ingredients, professional polishing agents may be 20 times more abrasive to dentin and ten times more abrasive to enamel than the polishing agents found in commercial toothpastes.1”
1. Darby, M. (2012). An Evidence-Based Approach to Polishing Teeth. American Academy for Oral-Systemic Health. Retrieved from http://aaosh.org/evidence-based-approach-cleansing-polishing-teeth/.
Exposed dentin is 20 times more susceptible to polishing abrasion than enamel, with cementum being the most susceptible to polishing. Demineralized white spot lesions abrade three times more than normal enamel.
“Some dental surfaces can be damaged by polishing. Demineralized white spot lesions abrade three times more than normal enamel. Additionally, stronger outer enamel may cover a decalcified inner layer. Removal of this outer layer can expose the more vulnerable layer beneath. Exposed dentin is 20 times more susceptible to polishing abrasion than enamel. Cementum, the least mineralized dental tissue, is obviously the most susceptible. It is interesting to note that cemental abrasion increases exponentially as rotational speed is increased. Dental materials such as gold and composite can also be scratched by polishing. Clinicians should take care when polishing any of the aforementioned surfaces, consider the benefits and risks and choose appropriate pressure, speed, and agents for the surfaces that are polished.1”
1. Pence, S.D., et al. (2011). Repetitive Coronal Polishing Yields Minimal Enamel Loss. The Journal of Dental Hygiene. 85(4): 348-357. Retrieved from http://jdh.adha.org/content/jdenthyg/85/4/348.full.pdf.
A prophy angle’s rubber cup type does not contribute to the quality of the polishing procedure.
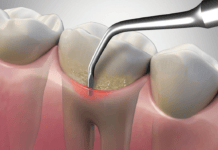
Prophy angle rubber cup type does contribute to the quality of the polishing procedure. Cup type and design impact the amount of agent applied to the tooth surface while polishing. Webbed prophy angle cups retain less paste than ribbed cups, which reduces abrasiveness.1
The firmer the rubber cup, the more pressure is needed to flare the cup against the tooth. Excessive pressure can increase the risk of tooth abrasion. Also, many manufacturers recommend operating handpieces at 3,000 rpm, with contact time per tooth being between 1-2 seconds.2
1. Gladwin M, Bagby M. Clinical Aspects of Dental Materials. 4th. Philadelphia: LWW; 2013:205–220.
2. Darby, M. (2012). An Evidence-Based Approach to Polishing Teeth. American Academy for Oral-Systemic Health. Retrieved from http://aaosh.org/evidence-based-approach-cleansing-polishing-teeth/.