The risk associated with cross-contamination while cleaning dental appliances is a topic that has garnered more attention in recent years. During a dental hygiene appointment, we are tasked with thoroughly cleaning our patients’ night guards, orthodontic appliances, and whitening trays at intermittent times throughout the day.
While the hygiene appointment is a balancing act, and we are often watching the clock while accomplishing multiple tasks, it’s important not to rush this portion of the visit. The reason for this is twofold:
- Primarily, we want to ensure that all debris is removed from the appliance and that it is returned to the patient in good condition (and if an appliance is given to us covered in debris, it can be a perfect opportunity to pivot into home care instruction).
- Equally as important, though, we want to ensure that we don’t facilitate a breach in infection control and place our patients at risk.
Current Practices
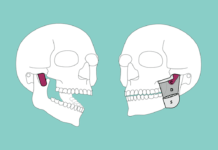
At the start of a hygiene visit, most offices clean dental appliances by placing them in a mixture of stain and tartar remover (or chemical tablets) and water in a sealed sandwich bag. This bag is then placed into an ultrasonic machine, and the vibrations from the ultrasonic help to loosen debris and leave an appliance with a sleeker, shinier look. This process typically occurs during our instrumentation. The appliance is then removed from the machine, rinsed with water, brushed to ensure complete debris removal, and returned to the treatment room (with many opportunities for the doctor to inspect it and ensure that it fits properly).
However, there is much to be said about the way that the cleaning of appliances is performed, and it is imperative that we think critically about preventing cross-contamination.
Separation of Ultrasonic Solutions
Not all practices separate the ultrasonic that is used to clean dental instruments from the ultrasonic that is used to clean patient appliances. This can lead to serious cross-contamination that not only violates infection control but also places our patients at risk for ingesting potentially harmful bacteria.
When our primary ultrasonic unit is used to clean sharp instruments throughout a busy day, and then (sometimes multiple) providers place plastic bags on top of these instruments, it creates the potential for instruments to puncture the bags, enabling bacteria from both items to come into contact with one another.
Likewise, the solution from the encased dental appliance can also leak out of the top of the bag and spill into the ultrasonic machine. Are we really leaving patients better than we found them if we are setting them up to encounter bacteria from other procedures? While these scenarios do not always play out in the worst way, it’s our responsibility as providers to follow all best practices during our patient care.
Some Solutions (Pun Intended)
There are several ways that we can clean our patients’ appliances and ensure that we are following the best guidelines. First, we can make the case for better infection control and encourage our employers to purchase a small, separate ultrasonic cleaner that can be used just for appliances. Additionally, an alternate lid for the primary ultrasonic and two small beakers can be used. When placed appropriately, this can keep our appliances separated from the instruments below them even though the two items are being cleaned in tandem.
It bears repeating that those who are in our care look to dental hygienists to advocate for their oral health, guiding them toward optimal health. The public places a great deal of trust in us and often uses us a model for bringing their health into balance. By using stricter infection control practices when cleaning appliances, we can truly continue to provide the best care to our patients.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.