I am a new dental hygienist, licensed for about four months now. I see a lot of patients for periodontal maintenance. My concern with some more involved perio patients I’m running into is, during periodontal probing there isn’t a huge difference from the previous charting. Their pocket depths are ranging from 4-7 mm, OH is poor/fair, and it seems the disease is still active. They have been on this maintenance for a while, a couple years or so. Should SRP be re-recommended depending on when it was done previously?
Also, would this type of patient always be on periodontal maintenance recall due to the depth of the pockets, since a prophylaxis is supragingival? Lastly, if after the SRP is re-done, and there still is no sign of a positive outcome, what would you recommend to the patient?
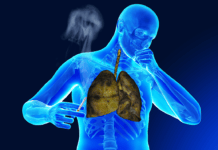
If a perio maintenance patient, or any patient, presents with active disease, 4-7 mm pockets, along with clinical attachment loss, non-surgical periodontal therapy/SRP is warranted. Remember there are more factors to consider than just pocket depths. You want to treat the patient based on their periodontal condition, not based on what the insurance covers. Make sure you explain to the patient what periodontal disease is, what causes it, what could happen if the appropriate treatment doesn’t take place, alternative treatment, and home care options that can help them. This is also a good time to educate patients on the oral-systemic link. For a good explanation of periodontal treatment protocol from the Journal of Dental Hygiene click here. On a side note, this was written before the gingivitis code, D4346, was implemented.
After definitive periodontal treatment, a patient is put on perio maintenance. Patients aren’t put on perio maintenance necessarily due to pocket depths, but because they are now in a state of “maintenance” of disease, not “prevention” of disease. Perio maintenance patients are put on a more frequent recall than a prophy patient because of how quickly virulent bacteria can form. The goal is to keep virulent, pathogenic, disease-causing bacteria at bay.
According to the ADA, how long a patient stays on perio maintenance is up to the clinical judgment of the dentist. The ADA states, “This is a matter of clinical judgment by the treating dentist. Follow-up patients who have received active periodontal therapy (surgical or nonsurgical) are appropriately reported using the periodontal maintenance code D4910. However, if the treating dentist determines that a patient’s oral condition can be treated with a routine prophylaxis, delivery of this service and reporting with code D1110 may be appropriate.” (CDT 2009/2010 page 157) So, while many perio patients will need perio maintenance for a lifetime, there is some discretion given for dentists to return a patient to prophy status. Meaning, if a perio maintenance patient has been periodontally stable for a few years, according to the ADA, they can be put back to prophy status if the dentist deems it appropriate.
To clarify, when performing a prophy, you want to scale subgingivally to the base of the sulcus. Bacteria form both supragingivally and subgingivally, with the most virulent bacteria being subgingival. For a prophy to be therapeutic, all biofilm and calculus must be removed. Click here for a Position Paper on prophylaxis from the ADHA.
If periodontal treatment has been completed, and the patient’s periodontal condition isn’t improving, tightening up their recall schedule is an option. For instance, instead of 4 months, maybe the recall should be 2-3 months. If a patient isn’t improving, it might also be time to refer them to a periodontist. It may not be improving due to lack of motivation, lack of homecare, systemic conditions, among other factors. Recognizing the disease-causing factors for each patients’ individual situation then treating, educating, and making referrals based on that, will hopefully bring your patients back to health.
SEE ALSO: Ground Breaking Perio Vaccine May Begin Trials in 2018