Total joint replacements are surgical procedures that replace a damaged or arthritic joint with a prosthetic joint. This procedure is common knowledge among the public and, most certainly, among dental professionals. According to the American Academy of Orthopedic Surgeons, the hip and knee are among the most commonly replaced joints.1 While not as common, other joints such as the ankle, wrist, shoulder, and elbow can also be replaced. However, did you know that the temporomandibular joint (TMJ) can also be replaced?
The History of TMJ Replacement
In 1840, Dr. John Murray Carnochan, a New York surgeon, attempted to mobilize an ankylosed mandible by placing a small block of wood between the raw bony surfaces after resection of the condylar neck.2 However, the first official TMJ total joint replacement (TMJR) dates back to the 1960s.3 This joint replacement has evolved since then, including the materials used.
Initially, reports of adverse side effects left many believing that temporomandibular joint replacement was not possible. Comprised of vitreous carbon, aluminum oxide, synthetic hydroxyapatite, and polytetrafluoroethylene, the Proplast-Teflon device was used in approximately 26,000 patients by the late 1980s.4
Unfortunately, many patients reported irreversible and life-altering symptoms related to a mechanical failure resulting in soft tissue damage and foreign body giant cell reaction. In January 1991, the US Food and Drug Administration (FDA) ordered this implant to be removed from the market.4
Currently, there are three main TMJ prosthetic systems in use that are FDA approved: a patient-fitted or custom TMJ replacement system manufactured by TMJ concepts, a stock replacement by Zimmer Biomet, and a stock and custom fit by Nexus CMF.2,5 Zimmer Biomet also manufactures a custom TMJ replacement system that has yet to be approved by the FDA for use in the United States.5
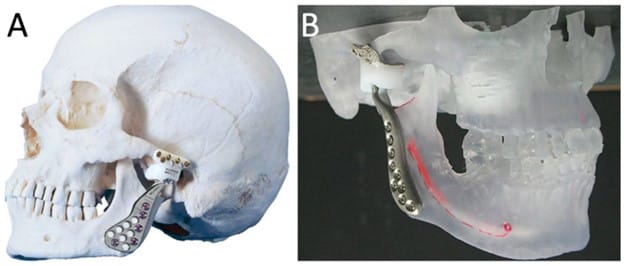
Image courtesy Pinto-Borges, H., et al.6
(CC BY 4.0 DEED)
All of these systems use materials such as Cobalt-Chrome-Molybdenum or Titanium condylar components with ultrahigh molecular weight polyethylene-based fossa components that have been used for decades in successful orthopedic joint replacements.5
Patient Eligibility for TMJ Replacement
Those who would be possible candidates for TMJ replacement include:7
- Those who have previously undergone TMJ surgical treatment that has failed
- Those who have undergone unsuccessful non-surgical treatment
- Patients who have had inflammatory or immunological responses, including end-stage TMJ deterioration
- Patients with severe pain and/or limited function
- Those with severe trauma to the TMJ, deformities, arthritis, tumors, ankylosis, or other issues that would render the joint dysfunctional
There are only a few circumstances that would absolutely contraindicate a TMJ replacement, such as patients with active infections and those who are allergic to the implant materials.5
TMJ Replacement Protocol
Those who choose to proceed with the surgery will have a thorough pre-surgical workup that includes CT scans, radiographs, bite registrations, maxillary and mandibular impressions, and clinical analysis. Some surgeons may use a 3-dimensional stereolithographic model of the TMJ created from the scans to fabricate the custom prosthesis and perform a mock surgery to ensure surgical success.5
The surgeon will then replicate the exact modifications performed in the mock surgery on the patient during the actual procedure to ensure a sufficient gap has been created between the base of the skull and ramus and that an adequate amount of the coronoid process has been removed. However, technology has allowed even more precision with computer-aided virtual surgical planning (VSP). This technology allows the surgeon to create a precise plan before surgery using technology without a physical 3D model.5
It should also be noted that approximately two-thirds of patients could benefit from orthognathic surgery concurrently. These particular patients will have better chewing and opening and enhanced airway/breathing following the combination of TMJR and orthognathic surgery. A custom device better serves those undergoing orthognathic surgery for a more precise fit and facilitates the correction of dentofacial deformities with greater accuracy and speed.8
Finding a surgeon who is qualified to perform the surgery may be a feat in itself. A study on oral and maxillofacial surgery resident training and exposure to TMJ replacement revealed that only 25% of responding programs admitted to only doing 10 or more cases annually. Studies indicate that by 2030, 902 (58% increase) TMJR surgeries will be completed in the United States alone.5
Post Procedure
Healing time can take approximately 12 weeks, and post-op procedures vary by doctor. Some common post-op care includes:9
- Patients are given pain management prescriptions and antibiotics for a week to prevent infections.
- Intraoral elastics are placed to help guide the mandible movement for the first week.
- During this week, a liquid diet will be necessary. Once the elastics are removed, a soft, no-chew diet will be implemented for six to eight weeks.
- Physical therapy is typically started one week after surgery, as not moving increases the chance of non-optimal surgical results.
- The treating surgeon may require pre-medication for dental visits for a length of time following a TMJR, if necessary.
Considering that a patient’s jaw is immobilized and banded together with elastics for a brief period of time, oral hygiene will present challenges, especially for the lingual surfaces of the teeth. Patients should always seek advice on dental hygiene care from their surgeon. However, dental professionals can help explain the importance of maintaining good oral hygiene regimens.
An overview of TMJR post-op instructions includes:10,11
- Gentle brushing with a child-size toothbrush can begin the first day following surgery. Teeth should be brushed at least three times per day, particularly after each meal.
- It may be difficult to brush teeth until the swelling subsides and the elastics are removed. Using the prescribed mouth rinse (i.e., CHX) or saltwater rinses will help provide oral hygiene during the first week following surgery. It is ideal to rinse after eating, if possible. If not, rinse at least three times per day.
- Mouth rinse should not be vigorously swished the first week following surgery if TMJR is combined with upper jaw surgery or genioplasty, as this may harm incisions. Instead, swish gently or place mouth rinse in the mouth and roll the head around for 30 seconds.
- Do not use a water flosser or electric toothbrush for seven to 10 days following surgery, as they can cause problems if used too early.
My Patient’s Story
Many years ago, at my patient’s first examination, it was evident that her opening was very limited. She informed me that as a young child, around the age of seven, she hit her jaw on the edge of her swimming pool, which stunted the growth of her mandible. At 16 years old, she still had the mandible of a seven-year-old, which led to her journey for surgical correction.
She sought treatment from a doctor who held both Doctor of Dental Surgery (DMD) and Doctor of Medicine (MD) degrees and did his residency in oral and maxillofacial surgery. He was one of the founders of the American Society of TMJ Surgeons. He is also accredited with many major advancements in the field of temporomandibular joint disorders.
According to my patient, she became the first candidate in the United States to have this form of surgery to correct her mandible growth. He performed bilateral costochondral grafts using a graft of my patient’s rib bone.
Recently, I noticed her opening had become increasingly smaller. The normal range of mouth opening is 35 to 55 mm, but hers was 24 mm measured at the canines’ incisal edges. When questioned, she admitted to increased pain within the joint. A panoramic radiograph revealed severe deterioration in the TMJ.
It was then I made the suggestion that she seek a consultation with her surgeon. At the consult, it was discovered that over the course of the last 19 years, her rib grafts have resorbed and are showing signs of fibrous ankylosis.
She is now preparing for a bilateral TMJR with pre-operative orthodontics to help with mandible placement. Her surgeon is having a bilateral custom-made device fabricated to replace the original rib graft that takes months to create.
How Dental Professionals Can Help
I find it necessary to evaluate the TMJ area during routine dental appointments. This very simple and quick examination can help detect any issues and open a window of conversation about treatment.
With the patient seated in the dental chair, the clinician can place the fingers over the TMJ and slightly below the ear while the patient opens, closes, and moves the mandible from side to side several times. The clinician should note any crepitus, pain, shifting, and limited range of motion. Clinicians should then palpate the masticator muscles for any stiffness, knots, and tenderness.
During the intraoral examination, signs of bruxism should be evaluated, and deep or collapsed bites should be documented. Taking panoramic radiographs allows the clinician to evaluate the structural composition of the joint and note any malformations or obvious injuries.
In Closing
Dental professionals should be well educated on the TMJ to help assist patients who may be at risk or currently suffering from temporomandibular joint disorders. Having a wealth of knowledge to guide patients will help reduce or prevent further damage to an already complex joint.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Foran, J.R.H. (2021, February). Total Joint Replacement. American Academy of Orthopedic Surgeons. https://orthoinfo.aaos.org/en/treatment/total-joint-replacement/
- Mercuri, L.G. Temporomandibular Joint Replacement Devices – Dark Past to Challenging Future. Stomatological Disease and Science. 2019: 3: 3. https://doi.org/10.20517/2573-0002.2018.25
- De Meurechy, N.K.G., Zaror, C., Mommaerts, M.Y. Total Temporomandibular Joint Replacement: Stick to Stock or Optimization by Customization? Craniomaxillofacial Trauma and Reconstruction. 2020; 13(1): 59-70. https://doi.org/10.1177/1943387520904874
- Sinno, H., Tahiri, Y., Gilardino, M., Bobyn, D. Engineering Alloplastic Temporomandibular Joint Replacements. McGill Journal of Medicine. 2011; 13(1): 63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3277342/
- Dang, R.R., Mehra, P. Alloplastic Reconstruction of the Temporomandibular Joint. Journal of Istanbul University Faculty of Dentistry. 2017; 51(3 Suppl 1): S31-S40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5750826/
- Pinto-Borges, H., Carvalho, O., Henriques, B., et al. A Preliminary Analysis of the Wear Pathways of Sliding Contacts on Temporomandibular Joint Total Replacement Prostheses. Metals. 2021; 11(5): 685. https://www.mdpi.com/2075-4701/11/5/685
- Temporomandibular Joint (TMJ) Implants. (2021, July 7). US Food and Drug Administration. https://www.fda.gov/medical-devices/temporomandibular-disorders-tmd-devices/temporomandibular-joint-tmj-implants
- Amarista, F.J., Perez, D.E. Concomitant Temporomandibular Joint Replacement and Orthognathic Surgery. Diagnostics. 2023; 13(15): 2486. https://doi.org/10.3390/diagnostics13152486
- After TMJ replacement. (n.d.) Northeast Facial and Oral Surgery Specialists, LLC. https://www.nefoss.com/surgical-instructions/after-tmj-surgery/after-tmj-replacement/
- Postoperative Instructions. (n.d.). Larry M. Wolford, DMD, Oral and Maxillofacial Surgery. https://drlarrywolford.com/postoperative-instructions/
- Surgical Instructions: TMJ Total Joint Replacement. (n.d.). Arizona Jaw Surgery. https://www.azjawsurgery.com/surgical-instructions/tmj-total-joint-replacement/