Amyloidosis refers to a group of diseases that cause an increase of the amyloid proteins to build up in various organs. With this disease, the proteins become twisted, misshapen, and/or clumped together, which results in excessive protein buildup.1 Amyloidosis can be localized or generalized, both primary and secondary, as well as inherited.2-4
Dental professionals need to be aware of oral health complications, which are discussed below. For example, some oral manifestations that dental hygienists may observe could be the first visible indications of amyloidosis.
Causes and Types of Amyloidosis
Amyloid light chain (A-light chain or AL), also known as primary amyloidosis, is the most common systemic type of the disease. Light chains are part of the antibodies made by plasma cells. During this type of disease, plasma cells normally responsible for fighting infections in the body create too many light chains, which is considered abnormal. Due to the shape, the light chains fold over on themselves and coalesce together, which creates a buildup in various organs. This type predominantly affects the kidneys, liver, heart, skin, nerves, and stomach.1,4,5
The form amyloid serum A protein (AA or SAA) of amyloidosis is caused by a buildup of serum A in the body. Serum A proteins can build up if there is inflammation present in the body for an extended period. This type of amyloidosis is a secondary form of the disease directly associated with inflammation from other diseases or sources. Some examples of these causes can be inflammatory bowel disease, rheumatoid arthritis, and any long-standing infection. The organs that are typically affected by this variation are the liver, kidneys (most common), stomach, spleen, and intestines.1,4,6
The form amyloid transthyretin protein (TTR protein or ATTR) of amyloidosis can also be known as familial amyloidosis, indicating that it is an inherited form of the disease. The liver is responsible for making a protein called transthyretin (TRR), which transmits vitamin A and thyroid hormones within the blood. In this form of amyloidosis, the TRR protein breaks down, which creates small fibers to build up in nerves and the heart.1,4,7
In the heart, the protein deposits harden the left ventricle, making it more difficult for the heart to pump blood to the body. This can cause shortness of breath, heart palpitations, edema, and coughing/wheezing. When the amyloid deposits associated with ATTR build up in the nerves, patients often experience carpal tunnel, eye floaters, and peripheral neuropathy.7
With wild-type amyloidosis, previously known as senile systemic amyloidosis, the transthyretin protein that is also found in hereditary amyloidosis is also present in this case. With age, the TTR protein becomes unstable, making it prone to misfolding, leading to buildup in the heart. This usually affects men over the age of 60.8,9
Localized amyloidosis tends to affect the throat, bladder, skin, and lungs. This type usually has a good prognosis due to its localized disease tendencies.1,3
Amyloidosis Symptoms
The following are all possible signs and symptoms of amyloidosis:3,10
- Fatigue and exhaustion that is considered severe
- Unidentified weight loss
- Feeling short of breath
- Pain in the joints
- Skin that bruises easily
- Purple-colored skin around the eyes
- Gastrointestinal discomfort like diarrhea and/or constipation
- Enlarged, scalloped tongue
Amyloidosis Risk Factors and Complications
The most common age for diagnosis is between 60 and 70 years old. Men tend to be more affected by the disease compared to women. However, women tend to have a higher prevalence of oral symptoms. As discussed previously, various chronic infections or diseases as well as a familial history of the disease, can increase a person’s chance of developing amyloidosis. During dialysis, some proteins cannot be removed from a patient’s blood, which may put a person at a greater risk of developing amyloidosis.1-3,10
Because amyloidosis can damage all sensory, motor, and autonomic nerves, the disease can often lead to a degradation of the affected areas.10 Some of the complications that can arise from this are numbness that can cause great discomfort, balance issues, nausea and/or vomiting, constipation, diarrhea, unusual perspiration, abnormal heartbeats, and kidney failure.3-4,10
Amyloidosis Diagnosis and Treatment
Diagnosis of amyloidosis may be difficult since the signs and symptoms of the disease can vary greatly and can mimic complications found with other diseases. This delay in diagnosis can allow a patient’s disease to progress and cause further organ damage.3
Lab tests may check for abnormal protein counts in the blood and urine. Imaging such as computed tomography (CT) scan to look at various organs, and an echocardiogram to evaluate a person’s heart may be used for diagnosis purposes. A bone marrow aspiration and biopsy are used to identify the mutated protein causing the specific type of amyloidosis.1,3,10
While there is no cure for the disease, many treatments are available to help slow the progression and reduce a patient’s symptoms.1,3,10
Treatments vary greatly for amyloidosis based on which organs are affected, whether it is mild, moderate, or severe and whether it is systemic or localized. Treatments also vary from patient to patient, depending on which symptoms need managing. One of the primary goals of treatment is to slow the creation of amyloid proteins.1-3,10
In cases of secondary amyloidosis that another systemic disease has caused, these need to be treated and managed as well to help prevent disease progression.1,3,10
Some common medications used to help slow the progression of the disease and, ultimately, further organ damage are chemotherapy drugs, blood thinners, beta-blockers, diuretics, and medications classified as targeted therapies. These can include patisiran, inotersen, tafamidis, and filunisal.1-3,10
Surgical interventions also can be taken to treat amyloidosis. This can include blood stem cell transplant (cells are taken from a person’s own body and then replaced), organ transplant (the most common transplants are liver, kidneys, and heart), and dialysis. The goal of surgical intervention is to improve a patient’s quality of life and hopefully continue to slow the progression of the disease.2,3,10
Oral Implications of Amyloidosis
Oral amyloidosis is usually secondary to systemic amyloidosis and isn’t common. However, when it occurs, the most common site is the tongue. The condition can present itself as macroglossia (enlarged tongue), where scalloping may occur on the lateral borders and/or with nodular, ulcerative lesions. Lesions may also appear purplish and hemorrhagic or papular, whitish or yellow.2,3
Beyond the tongue, oral manifestations such as lesions and edema can also occur in other areas of the mouth. These areas may include the lip, palate, gingiva, buccal mucosa, submandibular gland region, parotid gland region, floor of the mouth, palatine tonsils, uvula, or mandibular condyle.2
Patients may report oral symptoms such as dysgeusia (altered taste), dysphagia (swallowing difficulty), dysarthria (speaking difficulty), hoarseness, airway obstruction, xerostomia, and jaw claudication.2 Jaw claudication causes soreness, pain, and fatigue that often presents itself while talking and chewing. Once the patient stops these activities, the pain is resolved.2,4,11,12
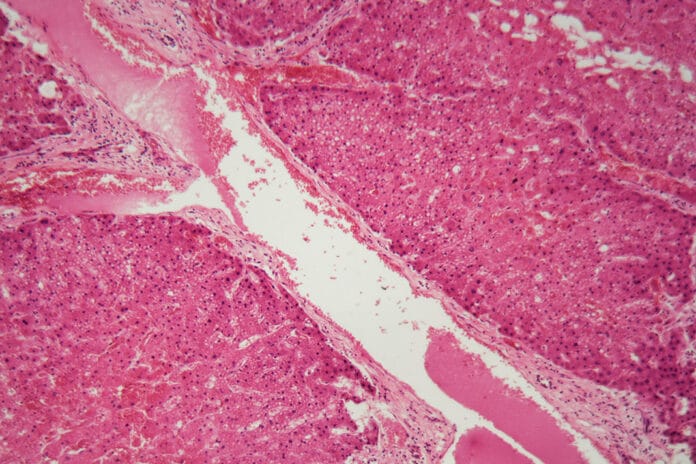
Like many other lesions and conditions found in the mouth, a biopsy continues to be considered the best tool and standard to diagnose this type of disease.2 “The histopathological analysis using Congo red staining is considered the gold standard for diagnosis because fibrillar protein deposits show green-yellow birefringence on polarized light.”2
A potential diagnosis of amyloidosis should be considered in cases of macroglossia with tongue ulcerations. As hygienists, we need to be aware of this disease because macroglossia may be the only visible symptom these patients present with.13
Why Hygienists Should Be Familiar with Amyloidosis
Dental hygienists are well-versed in many different, complex, systemic diseases and disorders. Our knowledge is not limited to those confined to the oral cavity. This is yet another example of how we can be the first line of defense in keeping our patients healthy and educated and proves how hygienists may be the first ones to notice when something is abnormal.
Understanding how systemic diseases present in the mouth and educating our patients so that they can seek prompt medical treatment is one of the key components of practicing as a hygienist. As previously stated, amyloidosis can progress due to lack of treatment, so if we can spot the signs early, we may be able to help them get the care they need more promptly.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Amyloidosis. (2022, June 24). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23398-amyloidosis
- Pontes, F.S., Ferreira, G.B., Fonseca, F.P., et al. Oral Amyloidosis: An Update. Med Oral Patol Oral Cir Bucal. 2023; 28(4): e341-e346. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10314358/
- Mayo Clinic Staff. (2023, May 13). Amyloidosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/amyloidosis/symptoms-causes/syc-20353178
- Vaxman, I., Gertz, M. When to Suspect a Diagnosis of Amyloidosis. Acta Haematol. 2020; 143(4): 304-311. https://karger.com/aha/article/143/4/304/15394/When-to-Suspect-a-Diagnosis-of-Amyloidosis
- AL Amyloidosis (Primary Amyloidosis). (2022, June 24). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15718-amyloidosis-al-amyloid-light-chain
- AA Amyloidosis. (2022, June 23). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17854-amyloidosis-aa
- Transthyretin Amyloidosis (ATTR-CM). (2022, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17855-amyloidosis-attr
- Bustamante, J.G., Zaidi, S.R.H. (2023, July 31). Amyloidosis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK470285/
- Wild-Type Amyloidosis. (n.d.). Amyloidosis Research Consortium. https://arci.org/about-amyloidosis/wild-type-amyloidosis/
- Amyloidosis. (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/amyloidosis
- Palladini, G., Merlini, G. How I Treat AL Amyloidosis. Blood. 2022; 139(19): 2918-2930. https://ashpublications.org/blood/article/139/19/2918/476883/How-I-treat-AL-amyloidosis
- Syed, A. (n.d.). Jaw Claudication: What Is It, Causes, Diagnosis, and More. Elsevier. https://www.osmosis.org/answers/jaw-claudication
- Kutti Sridharan, G., Rokkam, V.R. (2023, August 8). Macroglossia. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK560545/