We all know that children need to have the best, most positive dental experience to ensure a fondness for a lifetime of dental visits. We want to help eliminate stress and apprehension for both the clinician, patient, and their families. The best way to accomplish this is to start early.
With all expecting patients, take a few moments to discuss an early examination of pediatric dental patients, following the American Academy of Pediatric Dentistry’s (AAPD) recommendation of the first visit when the first tooth erupts or by the first birthday.1
The AAPD states, “The first examination is recommended at the time of the eruption of the first tooth and no later than 12 months of age.” They recommend this because “It has been reported that the number and cost of dental procedures among high-risk children is less for those seen at an earlier age versus later, confirming the fact that the sooner a child is seen by a dentist, the less treatment needs they are likely to have in the future. On the other hand, delayed diagnosis of dental disease can result in exacerbated problems which lead to more extensive and costly care.”1
The AAPD’s components of a comprehensive oral exam include assessment of:1
- General health/growth
- Pain
- Extraoral soft tissues
- Temporomandibular joints
- Intraoral soft tissues
- Oral hygiene and periodontal health
- Intraoral hard tissues
- Developing occlusion
- Caries risk
- Behavior of child1
More information about fluoride recommendations, radiographs, sealants, etc., can be found on the AAPD’s website.2
It’s best to start the conversation early so parents begin to think about their child’s future oral health and the importance of home care. By offering full home-care instructions and setting the stage for excellent health and compliance, we can add value to the dental appointment by educating parents.
Meeting a Child Patient
The first appointment is education-focused and should be fun and informative. It’s what we do best. Keep it low-key and positive, offering lots of praise and direction to both parent and child. Knee-to-knee examinations during the first examination tend to be most successful. Have the parent hold their child with the child’s legs wrapped around their waist and the head by their knees. This allows you to be knee-to-knee with the parent with full access to the child’s head and neck.
Examine all soft tissues, check for potential tongue and lip ties, eruption pattern anomalies, and access the teeth. Use Tell-Show-Do, meaning tell what you are planning to do, show the tools required, (i.e., mirror, explorer), and then do.
Try counting the parent’s fingers, then the child’s fingers gently with the back end of the explorer, then enter the mouth. This pattern instills confidence in the parent that their child is completely comfortable, even if they may be crying or squirming about. During this entire experience, discuss what you see, what you expect to see, and discuss any potential issues found and possible treatment options.
Get that super soft infant brush out and do a full toothbrush demonstration in the child’s mouth so that it can easily be recreated at home. Allow the parent to take the brush and practice with you so they can confidently create a plaque-free mouth at home. How can we expect a parent to brush if we have not given them the tools and knowledge?
Bumpy, Outside, Inside, Tongue
For brushing simplicity, teach the BOIT method (bumpy, outside, inside, tongue).3 This method was developed through a grant-funded program on oral health initiatives at Little City in Palatine, Illinois. Through a four-year grant and over 10,000 brushings, this method was shown to be easily reproducible and is now used in multiple states and various settings, including home, residential care, nursing homes, and hospitals. Wet the brush, apply a rice-sized portion of paste/gel or just water if sensory issues are noted, and increase to a pea-sized amount at age three. Try different flavors to add fun and increase interest in brushing.
The BOIT method is simple and easily reproducible. Start in the upper right and brush all occlusal maxillary teeth, drop to the mandibular left and brush all occlusal mandibular teeth. This creates one full circle of the bumpy biting surface (occlusal), or the B in BOIT. By brushing the bumpy/occlusal first, you have spread the toothpaste ensuring all surfaces have contact and adequate time in contact with the fluoride.
Next, in the same pattern of starting in maxillary right and ending in the mandibular right, brush the outsides, the facial surfaces, or the “parts you see when you smile.”
With the same pattern, then brush the insides, the linguals, or the “parts your tongue feels.” This pattern makes three complete circles, bumpy-occlusal, outsides-facials, and insides-lingual. Finally, instruct the parent to brush the tongue.
Until expectorating can be successful, a cloth can be used to wipe away excess saliva and paste.
Discuss Drinking with Parents
Also, be sure to discuss hidden sugars and the adverse reaction from sleeping with a bottle or sippy style cup. Many parents believe that if a product is labeled “organic” or “non-GMO,” it is healthy and not a dental issue.
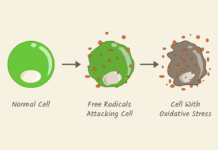
Clearly, we know this is far from true as it relates to tooth decay—stress water as being the only beverage allowed between meals. Discuss carbohydrates and sugars and how it relates to tooth decay.
This is easiest to do for many with some common food packages, perhaps a yogurt and 100% fruit juice. Point to the carbohydrates explaining that four grams of sugar equal one teaspoon of sugar. Showing the package and the volume of sugar is extremely effective! Point out the stickiness of raisins, candies, and granolas adhering to the “bumpy surfaces,” and sticking the sugars to the teeth causes an increased risk of tooth decay.
If the appointment is progressing nicely and time allows, demonstrate the use of the prophy angle. Again, use Tell-Show-Do. Let parent and child listen to the sound, feel the rubber cup on a finger as well as possibly on the tooth if the child allows it. Perhaps try to gently polish with a bit of prophy paste after allowing both parent and child to smell it.
Apply a fluoride varnish sparingly at the conclusion of the appointment. Base the appointment flow and treatment on behavior and comfort of both parent and child.
We know the most important aspect of the initial appointment is education in their child’s oral health. Establishing confidence in the dental office team and a feeling of comradery sets everyone up for success! Explain the importance of primary teeth as not being simply “practice teeth” but necessary for speech, eating, and future permanent dentition eruption.
Offer a written pamphlet or sheet outlining BOIT brushing, frequency, basic nutrition with examples, and a reminder for a six-month return visit or sooner as needed. The AAPD offers many exceptional resources for both parents and clinicians on their website and has multiple brochures that can be downloaded and distributed.
Offer lavish praise for bringing the child to you for treatment and offer a sincere thank you for putting their trust in you. Creating a happy visit sets parents and the child up for a successful dental experience moving forward and eases potential apprehension. As dental professionals, we have the ability to help our youngest patients have the best experience and make dentistry joyful ─ a win for all!
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Periodicity of Examination, Preventive Dental Services, Anticipatory Guidance/Counseling, and Oral Treatment for Infants, Children, and Adolescents. (2018). American Academy of Pediatric Dentistry. Retrieved from https://www.aapd.org/research/oral-health-policies–recommendations/periodicity-of-examination-preventive-dental-services-anticipatory-guidance-counseling-and-oral-treatment-for-infants-children-and-adolescents/
- Oral Health Policies and Recommendations (The Reference Manual of Pediatric Dentistry). (2019. American Academy of Pediatric Dentistry. Retrieved from https://www.aapd.org/research/oral-health-policies–recommendations/
- CDT 2021 Coding Companion: Training Guide for the Dental Team. (2021). American Dental Association.